HHS ensures consumers get better value for their health insurance dollar
HHS ensures consumers get better value for their health insurance dollar
Administration actions saved consumers up to $323 million
Health and Human Services Secretary Kathleen Sebelius announced today that consumers will soon begin receiving unprecedented information on the value of their health insurance coverage, and some will receive rebates from insurance companies that spend less than 80 percent of their premium dollars on health care.
The Affordable Care Act requires that insurance companies this year begin notifying customers how much of their premiums they have spent on medical care and quality improvement. Beginning in 2011, insurers were required to spend at least 80 percent of total premium dollars they collect on medical care and quality improvement. Insurance companies that do not meet the 80/20 standard (also known as the Medical Loss Ratio) are required to pay rebates to their customers this year.
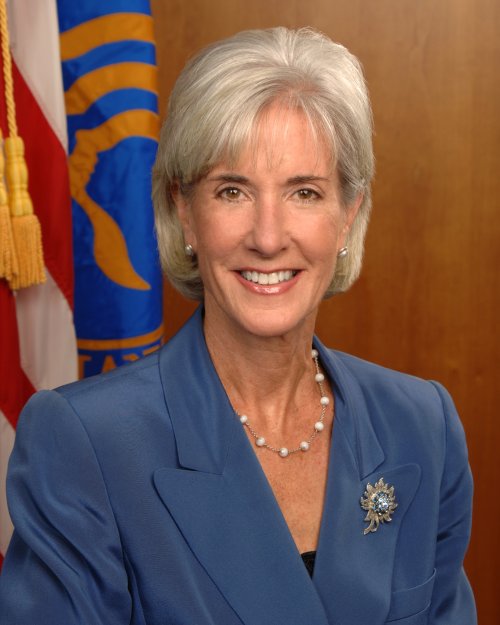
“Before the Affordable Care Act, insurance companies could spend your premium dollars on administrative red tape and marketing,” said Secretary Sebelius. “With today’s notice, we’re taking a big step toward making insurers accountable to consumers. Some of these insurance companies have already changed their behavior by lowering premiums or spending more on medical care and quality improvement, while the remainder will need to refund this money to their customers this year.”
The proposed consumer notices about whether their insurance company has met the new standard have been posted on HealthCare.gov, and HHS is seeking public comment to help ensure the notices are useful transparency tools for consumers.
In the individual market, the Affordable Care Act allows the Secretary to adjust the medical loss ratio standard for a state if it is determined that meeting that standard may destabilize the state’s individual insurance market. HHS has concluded its review of 18 state requests for adjustments to the medical loss ratio rule. As a result of HHS’ decision to deny insurance companies the ability to spend more premium dollars on administrative overhead costs rather than on medical claims, consumers will receive up to $323 million in rebates this year compared to what would have been owed if all state adjustment requests were fully granted, according to data from state regulators and issuer reports.
These adjustment request determinations were made as a result of a transparent and data-driven process, and the documentation related to each state’s request has been publicly posted. In total, HHS determined that no adjustment was necessary in ten states, approved an altered adjustment in six states, and approved the request sought by one state. This includes a denied adjustment for Wisconsin, and an altered adjustment for North Carolina, both announced today.
Today’s announcement is part of the Obama Administration’s effort to increase transparency in the health insurance marketplace. The notification will let consumers know if their insurer did not meet the 80/20 standard — and that they or their employer will receive a rebate. HHS is also considering requiring insurers notify consumers if their insurer did meet the 80/20 standard.
For the text of these proposed notifications, please visit: http://cciio.cms.gov/resources/other/index.html#mlr
###
Medical Loss Ratio: Getting Your Money’s Worth on Health Insurance
Today, many insurance companies spend a substantial portion of consumers’ premium dollars on administrative costs and profits, including executive salaries, overhead, and marketing. Thanks to the Affordable Care Act, consumers will receive more value for their premium dollar because insurance companies will be required to spend 80 to 85 percent of premium dollars on medical care and health care quality improvement, rather than on administrative costs, starting in 2011. If they don’t, the insurance companies will be required to provide a rebate to their customers starting in 2012.
On November 22, 2010, the Obama Administration issued a regulation implementing this policy, known as the “medical loss ratio” provision of the Affordable Care Act. This regulation will make the insurance marketplace more transparent and make it easier for consumers to purchase plans that provide better value for their money.
Over 20 percent of consumers who purchase coverage in the individual market today are in plans that spend more than 30 cents of every premium dollar on administrative costs. An additional 25 percent of consumers in this market are in plans that spend between 25 and 30 cents of every premium dollar on administrative costs. And in some extreme cases, insurance plans spend more than 50 percent of every premium dollar on administrative costs. This regulation will help consumers get good value for their health insurance premium dollar.
In 2011, the new rules will protect up to 74.8 million insured Americans, and estimates indicate that up to 9 million Americans could be eligible for rebates starting in 2012 worth up to $1.4 billion. Average rebates per person could total $164 in the individual market. Important details regarding the new regulation are included below.
How These New Rules Will Help You – Ensuring Value for Consumers
The new medical loss ratio rules will hold insurance companies accountable and increase value for consumers by:
- Establishing Greater Transparency and Accountability: Beginning in 2011, the law requires that insurance companies publicly report how they spend premium dollars. This information will provide consumers with meaningful information on how their premium dollars are spent, clearly accounting for how much money goes toward actual medical care and activities to improve health care quality versus how much money is spent on administrative expenses like marketing, advertising, underwriting, executive salaries and bonuses.
- Ensuring Americans Receive Value for their Premium Dollar: Beginning in 2011, the law requires insurance companies in the individual and small group markets to spend at least 80 percent of the premium dollars they collect on medical care and quality improvement activities. Insurance companies in the large group market must spend at least 85 percent of premium dollars on medical care and quality improvement activities.
- Providing Rebates to Consumers: Insurance companies that are not meeting the medical loss ratio standard will be required to provide rebates to their consumers. Insurers will be required to make the first round of rebates to consumers in 2012. Rebates must be paid by August 1st each year. Enrollees owed a rebate will see a reduction in their premiums, receive a rebate check, or, if the enrollee paid by credit card or debit card, a lump-sum reimbursement to the same account that the enrollee used to pay the premium. In some cases, the rebate may go to the employer that paid the premium on the enrollee’s behalf. Regardless of whether the rebate is provided to enrollees directly or indirectly through their employer, each enrollee must receive a rebate that is proportional to the premium amount paid by that enrollee.
Working with State Experts: Developing the Medical Loss Ratio Regulation
The Affordable Care Act required the National Association of Insurance Commissioners (NAIC) to develop uniform definitions and methodologies for calculating insurance companies’ medical loss ratios. Insurance commissioners in every State have a responsibility to protect the interests of the general public, policyholders, and enrollees within their respective States. Today’s regulation certifies and adopts the recommendations submitted to the Secretary of Health and Human Services (HHS) on October 27, 2010, by the NAIC. It also incorporates recommendations from a letter sent to the Secretary by the NAIC on October 13, 2010. The NAIC report was approved unanimously by representatives from every State and the District of Columbia and is the product of months of public hearings and consultation with consumers, employers, insurers, and other stakeholders. The NAIC has a long history of developing these types of rules through a transparent process with stakeholder input, and this process was no exception.
The medical loss ratio regulation outlines disclosure and reporting requirements, how insurance companies will calculate their medical loss ratio and provide rebates, and how adjustments could be made to the medical loss ratio standard to guard against market destabilization.
Insurer Reporting Requirements
Beginning in 2011, insurance companies that issue policies to individuals, small employers, and large employers will have to report the following information in each State it does business:
- Total earned premiums;
- Total reimbursement for clinical services;
- Total spending on activities to improve quality; and
- Total spending on all other non-claims costs excluding federal and State taxes and fees.
These reports will be posted publicly by HHS so residents of every State will have information on the value of health plans offered by different insurance companies in their State.
An insurer will report aggregate premium and expenditure data for each market, except for so-called “expatriate” and “mini-med” plans. For these plans, insurers will be allowed to report their experience separately. Although the NAIC did not make a formal recommendation on this subject, in their letter sent to Secretary Sebelius on October 13, 2010, the NAIC recommended that the Secretary exclude expatriate plans—health insurance provided to U.S. citizens who are living or working abroad – from the new requirements. The regulation accelerates data collection and creates a special methodology that follows this recommendation to the extent permitted by the Affordable Care Act. HHS is allowing the same treatment for mini-med plans — insurance products with very low annual dollar limits and low premiums – to allow this type of coverage to continue until 2014 when better, more affordable options will be available to consumers.
Activities That Improve Health Care Quality
Following NAIC recommendations, this regulation specifies a comprehensive set of “quality improving activities” that allows for future innovations and may be counted toward the 80 or 85 percent standard. Quality improving activities must be grounded in evidence-based practices, take into account the specific needs of patients and be designed to increase the likelihood of desired health outcomes in ways that can be objectively measured.
In order to maintain incentives for innovation, insurers will not be required to present initial evidence in order to designate an activity as “quality improving” when they first begin implementing it. However, to ensure value, the insurer will have to show measurable results stemming from the quality improvement activity in order to continue claiming that it does in fact improve quality.
Timing of Reporting and Rebates
The regulation generally requires health insurance companies to report to the Secretary by June 1 of each year. The first report, containing calendar year 2011 data, will be due in 2012, which gives insurers adequate time to make necessary reporting adjustments. Insurers will be required to make the first round of rebates to consumers by August 2012 based on their 2011 medical loss ratio. Under the regulation, expatriate and mini-med plans that report separately will be required to report data to the Secretary on an accelerated basis.
Treatment of Taxes in the Rebate Calculation
Consistent with NAIC recommendations, the regulation will allow insurers to deduct federal and State taxes that apply to health insurance coverage from an insurer’s premium revenue when calculating its medical loss ratio. As NAIC recommended, taxes assessed on investment income and capital gains will not be deducted from premium revenue. In the case of non-profit plans, assessments they are required to pay in lieu of taxes may be deducted.
Accommodations to Ensure Continued Access to Coverage by Consumers
In order to guard against market destabilization, the Affordable Care Act stipulates that the reporting requirements and methodologies for calculating the medical loss ratio “be designed to take into account the special circumstances of small plans, different types of plans, and new plans.”
- Smaller Plans. Consistent with NAIC recommendations, this regulation allows insurers to add to their medical loss ratio a “credibility adjustment” when the insurer’s medical loss ratio for a market within a State is based on less than 75,000 people enrolled for an entire calendar year. The credibility adjustment recommended by the NAIC and adopted in the regulation addresses the statistical unreliability of experience based on a small number of people covered. Specifically:
- An insurer that has less than 1,000 people enrolled for an entire calendar year lacks sufficient experience to calculate a reliable or meaningful medical loss ratio. The experience of these very small insurers cannot sufficiently confirm that they have or have not met the medical loss ratio standard, and as a result those insurers are deemed non-credible and will not be required to provide rebates.
- An insurer with 1,000 to 75,000 people enrolled for an entire calendar year is considered to have “partially credible” experience, and, accordingly, the regulation adds a “credibility adjustment” to its medical loss ratio.
- An insurer with 75,000 or more people enrolled in a plan for an entire calendar year is considered to have “fully credible” experience and will pay rebates based on its actual medical loss ratio without any credibility adjustment.
The NAIC commissioned an extensive analysis by a well-known national actuarial consulting firm, and relied on these findings to develop its credibility adjustment calculation. In developing its recommendations, the NAIC noted that the credibility adjustment methods and factors should be monitored and re-evaluated in light of developing experience. The Administration intends to carefully monitor the effects and suitability of the regulation’s initial approach to credibility adjustment over the next three years.
- Newer Plans. Consistent with NAIC recommendations, certain insurers that have newly joined the insurance market may be able to delay reporting their medical loss ratio until the next year. When 50 percent or more of an insurer’s premium income accounts for policies that have not been effective for an entire calendar, they are eligible to delay reporting until the following year. This means that more than half of an issuer’s overall premium revenue within a particular market in a State would have to be from policies that are newly issued policies after January 1 of the year. In this instance, the issuer’s MLR for the following year will include the deferred experience, as well as the current MLR reporting year experience.Allowing insurance companies to defer reporting newer business reduces barriers to market entry by reducing the risk of failing to meet the MLR standard and having to pay a rebate.
- Mini-Med and Expatriate Plans. In order to address the special circumstances of mini-med and expatriate plans, HHS will apply a methodological adjustment to the way the medical loss ratio is calculated for those plans. The methodological adjustment will address the unusual expense and premium structures of mini-med and expatriate plans, and enable their issuers to apply for an adjustment to reported medical claims and quality improvement expenses. Because limited data are available to inform such an adjustment, this regulation requires accelerated reporting by issuers of mini-med and expatriate plans so that HHS may receive and review data on their expense structures and profitability. These changes to the methodology for reporting and rebates apply only in calendar year 2011, and as noted above, such plans are required to provide early reporting to the Secretary if they claim such an adjustment. To improve transparency and ensure consumers are aware of the product they are purchasing, HHS will require insurers that sell mini-med policies to provide prominent notice regarding the benefits and coverage provided by the policy.
Accommodations to Avoid Market Destabilization
In the individual market, the Affordable Care Act allows the Secretary to adjust the medical loss ratio standard for a State if it is determined that meeting the 80 percent medical loss ratio standard may destabilize the individual market. Consistent with NAIC recommendations, the regulation establishes a process for States to request such an adjustment for up to three years – an effective State-based transition. In order to qualify for this adjustment, a State must demonstrate that requiring insurers in its individual market to meet the 80 percent MLR has a likelihood of destabilizing the individual market and could result in fewer choices for consumers.
The approach taken in the regulation is designed to give States and other interested parties full opportunity to present relevant information that the Secretary needs to make a timely determination about whether an adjustment to the statutory medical loss ratio standard is justified for insurers in that particular individual market. It is consistent with the recommendations in the NAIC letter dated October 13, 2010.
Enforcement
The Affordable Care Act gives the Secretary direct enforcement authority for the medical loss ratio requirements. However, HHS recognizes States’ capacity to assist in enforcement and will accept the findings of a State audit of MLR compliance if they are based on the medical loss ratio requirements set forth in federal law and regulations.
The regulation also requires insurers to retain documentation that relates to the data they reported and to provide access to those data and their facilities to HHS, so compliance with reporting and rebate requirements can be verified.
Finally, the regulation imposes civil monetary penalties if an insurer fails to comply with the reporting and rebate requirements set forth in the regulation, and it details the criteria and process for determining whether and in what amount such penalties should be imposed. Although the law allows HHS to develop separate monetary penalties for medical loss ratio non-compliance, HHS has adopted the HIPAA penalties in this regulation. The regulation’s penalty for each violation is $100 per entity, per day, per individual affected by the violation.
For more information on the MLR provision in the Affordable Care Act, please visit: http://www.healthcare.gov/news/factsheets/2010/11/medical-loss-ratio.html
###
Today, many insurance companies spend a substantial portion of consumers’ premium dollars on administrative costs and profits, including executive salaries, overhead, and marketing. Thanks to the Affordable Care Act, consumers will receive more value for their premium dollar because insurance companies will be required to spend 80 to 85 percent of premium dollars on medical care and health care quality improvement, rather than on administrative costs, starting in 2011. If they don’t, the insurance companies will be required to provide a rebate to their customers starting in 2012.
On November 22, 2010, the Obama Administration issued a regulation implementing this policy, known as the “medical loss ratio” provision of the Affordable Care Act. This regulation will make the insurance marketplace more transparent and make it easier for consumers to purchase plans that provide better value for their money.
Over 20 percent of consumers who purchase coverage in the individual market today are in plans that spend more than 30 cents of every premium dollar on administrative costs. An additional 25 percent of consumers in this market are in plans that spend between 25 and 30 cents of every premium dollar on administrative costs. And in some extreme cases, insurance plans spend more than 50 percent of every premium dollar on administrative costs. This regulation will help consumers get good value for their health insurance premium dollar.
In 2011, the new rules will protect up to 74.8 million insured Americans, and estimates indicate that up to 9 million Americans could be eligible for rebates starting in 2012 worth up to $1.4 billion. Average rebates per person could total $164 in the individual market. Important details regarding the new regulation are included below.
How These New Rules Will Help You – Ensuring Value for Consumers
The new medical loss ratio rules will hold insurance companies accountable and increase value for consumers by:
- Establishing Greater Transparency and Accountability: Beginning in 2011, the law requires that insurance companies publicly report how they spend premium dollars. This information will provide consumers with meaningful information on how their premium dollars are spent, clearly accounting for how much money goes toward actual medical care and activities to improve health care quality versus how much money is spent on administrative expenses like marketing, advertising, underwriting, executive salaries and bonuses.
- Ensuring Americans Receive Value for their Premium Dollar: Beginning in 2011, the law requires insurance companies in the individual and small group markets to spend at least 80 percent of the premium dollars they collect on medical care and quality improvement activities. Insurance companies in the large group market must spend at least 85 percent of premium dollars on medical care and quality improvement activities.
- Providing Rebates to Consumers: Insurance companies that are not meeting the medical loss ratio standard will be required to provide rebates to their consumers. Insurers will be required to make the first round of rebates to consumers in 2012. Rebates must be paid by August 1st each year. Enrollees owed a rebate will see a reduction in their premiums, receive a rebate check, or, if the enrollee paid by credit card or debit card, a lump-sum reimbursement to the same account that the enrollee used to pay the premium. In some cases, the rebate may go to the employer that paid the premium on the enrollee’s behalf. Regardless of whether the rebate is provided to enrollees directly or indirectly through their employer, each enrollee must receive a rebate that is proportional to the premium amount paid by that enrollee.
Working with State Experts: Developing the Medical Loss Ratio Regulation
The Affordable Care Act required the National Association of Insurance Commissioners (NAIC) to develop uniform definitions and methodologies for calculating insurance companies’ medical loss ratios. Insurance commissioners in every State have a responsibility to protect the interests of the general public, policyholders, and enrollees within their respective States. Today’s regulation certifies and adopts the recommendations submitted to the Secretary of Health and Human Services (HHS) on October 27, 2010, by the NAIC. It also incorporates recommendations from a letter sent to the Secretary by the NAIC on October 13, 2010. The NAIC report was approved unanimously by representatives from every State and the District of Columbia and is the product of months of public hearings and consultation with consumers, employers, insurers, and other stakeholders. The NAIC has a long history of developing these types of rules through a transparent process with stakeholder input, and this process was no exception.
The medical loss ratio regulation outlines disclosure and reporting requirements, how insurance companies will calculate their medical loss ratio and provide rebates, and how adjustments could be made to the medical loss ratio standard to guard against market destabilization.
Insurer Reporting Requirements
Beginning in 2011, insurance companies that issue policies to individuals, small employers, and large employers will have to report the following information in each State it does business:
- Total earned premiums;
- Total reimbursement for clinical services;
- Total spending on activities to improve quality; and
- Total spending on all other non-claims costs excluding federal and State taxes and fees.
These reports will be posted publicly by HHS so residents of every State will have information on the value of health plans offered by different insurance companies in their State.
An insurer will report aggregate premium and expenditure data for each market, except for so-called “expatriate” and “mini-med” plans. For these plans, insurers will be allowed to report their experience separately. Although the NAIC did not make a formal recommendation on this subject, in their letter sent to Secretary Sebelius on October 13, 2010, the NAIC recommended that the Secretary exclude expatriate plans—health insurance provided to U.S. citizens who are living or working abroad – from the new requirements. The regulation accelerates data collection and creates a special methodology that follows this recommendation to the extent permitted by the Affordable Care Act. HHS is allowing the same treatment for mini-med plans — insurance products with very low annual dollar limits and low premiums – to allow this type of coverage to continue until 2014 when better, more affordable options will be available to consumers.
Activities That Improve Health Care Quality
Following NAIC recommendations, this regulation specifies a comprehensive set of “quality improving activities” that allows for future innovations and may be counted toward the 80 or 85 percent standard. Quality improving activities must be grounded in evidence-based practices, take into account the specific needs of patients and be designed to increase the likelihood of desired health outcomes in ways that can be objectively measured.
In order to maintain incentives for innovation, insurers will not be required to present initial evidence in order to designate an activity as “quality improving” when they first begin implementing it. However, to ensure value, the insurer will have to show measurable results stemming from the quality improvement activity in order to continue claiming that it does in fact improve quality.
Timing of Reporting and Rebates
The regulation generally requires health insurance companies to report to the Secretary by June 1 of each year. The first report, containing calendar year 2011 data, will be due in 2012, which gives insurers adequate time to make necessary reporting adjustments. Insurers will be required to make the first round of rebates to consumers by August 2012 based on their 2011 medical loss ratio. Under the regulation, expatriate and mini-med plans that report separately will be required to report data to the Secretary on an accelerated basis.
Treatment of Taxes in the Rebate Calculation
Consistent with NAIC recommendations, the regulation will allow insurers to deduct federal and State taxes that apply to health insurance coverage from an insurer’s premium revenue when calculating its medical loss ratio. As NAIC recommended, taxes assessed on investment income and capital gains will not be deducted from premium revenue. In the case of non-profit plans, assessments they are required to pay in lieu of taxes may be deducted.
Accommodations to Ensure Continued Access to Coverage by Consumers
In order to guard against market destabilization, the Affordable Care Act stipulates that the reporting requirements and methodologies for calculating the medical loss ratio “be designed to take into account the special circumstances of small plans, different types of plans, and new plans.”
- Smaller Plans. Consistent with NAIC recommendations, this regulation allows insurers to add to their medical loss ratio a “credibility adjustment” when the insurer’s medical loss ratio for a market within a State is based on less than 75,000 people enrolled for an entire calendar year. The credibility adjustment recommended by the NAIC and adopted in the regulation addresses the statistical unreliability of experience based on a small number of people covered. Specifically:
- An insurer that has less than 1,000 people enrolled for an entire calendar year lacks sufficient experience to calculate a reliable or meaningful medical loss ratio. The experience of these very small insurers cannot sufficiently confirm that they have or have not met the medical loss ratio standard, and as a result those insurers are deemed non-credible and will not be required to provide rebates.
- An insurer with 1,000 to 75,000 people enrolled for an entire calendar year is considered to have “partially credible” experience, and, accordingly, the regulation adds a “credibility adjustment” to its medical loss ratio.
- An insurer with 75,000 or more people enrolled in a plan for an entire calendar year is considered to have “fully credible” experience and will pay rebates based on its actual medical loss ratio without any credibility adjustment.
The NAIC commissioned an extensive analysis by a well-known national actuarial consulting firm, and relied on these findings to develop its credibility adjustment calculation. In developing its recommendations, the NAIC noted that the credibility adjustment methods and factors should be monitored and re-evaluated in light of developing experience. The Administration intends to carefully monitor the effects and suitability of the regulation’s initial approach to credibility adjustment over the next three years.
- Newer Plans. Consistent with NAIC recommendations, certain insurers that have newly joined the insurance market may be able to delay reporting their medical loss ratio until the next year. When 50 percent or more of an insurer’s premium income accounts for policies that have not been effective for an entire calendar, they are eligible to delay reporting until the following year. This means that more than half of an issuer’s overall premium revenue within a particular market in a State would have to be from policies that are newly issued policies after January 1 of the year. In this instance, the issuer’s MLR for the following year will include the deferred experience, as well as the current MLR reporting year experience.Allowing insurance companies to defer reporting newer business reduces barriers to market entry by reducing the risk of failing to meet the MLR standard and having to pay a rebate.
- Mini-Med and Expatriate Plans. In order to address the special circumstances of mini-med and expatriate plans, HHS will apply a methodological adjustment to the way the medical loss ratio is calculated for those plans. The methodological adjustment will address the unusual expense and premium structures of mini-med and expatriate plans, and enable their issuers to apply for an adjustment to reported medical claims and quality improvement expenses. Because limited data are available to inform such an adjustment, this regulation requires accelerated reporting by issuers of mini-med and expatriate plans so that HHS may receive and review data on their expense structures and profitability. These changes to the methodology for reporting and rebates apply only in calendar year 2011, and as noted above, such plans are required to provide early reporting to the Secretary if they claim such an adjustment. To improve transparency and ensure consumers are aware of the product they are purchasing, HHS will require insurers that sell mini-med policies to provide prominent notice regarding the benefits and coverage provided by the policy.
Accommodations to Avoid Market Destabilization
In the individual market, the Affordable Care Act allows the Secretary to adjust the medical loss ratio standard for a State if it is determined that meeting the 80 percent medical loss ratio standard may destabilize the individual market. Consistent with NAIC recommendations, the regulation establishes a process for States to request such an adjustment for up to three years – an effective State-based transition. In order to qualify for this adjustment, a State must demonstrate that requiring insurers in its individual market to meet the 80 percent MLR has a likelihood of destabilizing the individual market and could result in fewer choices for consumers.
The approach taken in the regulation is designed to give States and other interested parties full opportunity to present relevant information that the Secretary needs to make a timely determination about whether an adjustment to the statutory medical loss ratio standard is justified for insurers in that particular individual market. It is consistent with the recommendations in the NAIC letter dated October 13, 2010.
Enforcement
The Affordable Care Act gives the Secretary direct enforcement authority for the medical loss ratio requirements. However, HHS recognizes States’ capacity to assist in enforcement and will accept the findings of a State audit of MLR compliance if they are based on the medical loss ratio requirements set forth in federal law and regulations.
The regulation also requires insurers to retain documentation that relates to the data they reported and to provide access to those data and their facilities to HHS, so compliance with reporting and rebate requirements can be verified.
Finally, the regulation imposes civil monetary penalties if an insurer fails to comply with the reporting and rebate requirements set forth in the regulation, and it details the criteria and process for determining whether and in what amount such penalties should be imposed. Although the law allows HHS to develop separate monetary penalties for medical loss ratio non-compliance, HHS has adopted the HIPAA penalties in this regulation. The regulation’s penalty for each violation is $100 per entity, per day, per individual affected by the violation.
###
Medical Loss Ratio
Background
Many insurance companies spend a substantial portion of consumers’ premium dollars on administrative costs and profits, including executive salaries, overhead, and marketing.
The Affordable Care Act requires health insurance issuers to submit data on the proportion of premium revenues spent on clinical services and quality improvement, also known as the Medical Loss Ratio (MLR). It also requires them to issue rebates to enrollees if this percentage does not meet minimum standards. MLR requires insurance companies to spend at least 80% or 85% of premium dollars on medical care, with the review provisions imposing tighter limits on health insurance rate increases. If they fail to meet these standards, the insurance companies will be required to provide a rebate to their customers starting in 2012.
The new law also directs the National Association of Insurance Commissioners (NAIC) to establish uniform definitions and standardized methodologies for determining what services constitute clinical services, quality improvement and other non-claims costs for carrying out this provision.
State Information
The law allows the Secretary to adjust the MLR standard for a state if it is determined that meeting the 80% Medical Loss Ratio standard may destabilize the individual market. In order to qualify for this adjustment, a state must demonstrate that requiring insurers in its individual market to meet the 80% MLR has a likelihood of destabilizing the individual market and result in fewer choices for consumers.
This HHS Bulletin describes the method and format states must use in order to apply for an MLR adjustment. Applications must be submitted by email to MLRAdjustments@hhs.gov.
- OCIIO Technical Guidance: Process for a State to Submit a Request for Adjustment to the Medical Loss Ratio Standard of PHS Act Section 2718 (December 17, 2010)
A state’s request for an adjustment to the MLR standard is a public document. The Secretary invites public comment regarding a state’s request. However, public comments must be submitted within 10 calendar days of HHS posting a state’s complete request online to guarantee consideration. The public comment period is designed to give all interested parties full opportunity to present relevant information to the Secretary, which will be considered in making a timely determination on whether an adjustment to the statutory MLR standard is justified for the state applicant’s individual market
For documentation of state requests for MLR adjustments, including specific information on rebates saved by HHS’ MLR adjustment determinations, visit: http://cciio.cms.gov/programs/marketreforms/mlr/index.html
###
Know the Facts, Know Your Rights
The Affordable Care Act: Increasing Transparency and Protecting Consumers
The Affordable Care Act includes new patient protections that give you greater control over your health care – as well as new resources to make the health care system more transparent and ensure you are receiving value for your health care dollars.
On December 9, 2010 the Department of Health and Human Services issued new rules that will give consumers more information about their health insurance plan. Under the new rules, health insurers offering “mini-med” plans must notify consumers in plain language that their plan offers extremely limited benefits and direct them to www.HealthCare.govwhere they can get more information about other coverage options. The rules require health plans with waivers to tell consumers if their health care coverage is subject to an annual dollar limit lower than what is required under the law. Specifically, the notice must include the dollar amount of the annual limit along with a description of the plan benefits to which the limit applies. HHS has also issued guidance restricting the sale of new mini-med plans except under very limited circumstances.
The Affordable Care Act will end “mini-med” plans in 2014 and provide Americans with affordable, high-quality coverage options. Unfortunately, today, mini-med plans are often the only type of private insurance offered to some workers. In order to protect coverage for these workers, HHS has issued temporary waivers from rules restricting the size of annual limits to some group health plans and health insurance issuers. Waivers only last for one year and are only available if the plan certifies that a waiver is necessary to prevent either a large increase in premiums or a significant decrease in access to coverage.
Key facts about the guidance issued on December 9 include:
- The consumer notice must include the dollar amount of the annual limit along with a description of the plan benefits to which the limit applies. This notice must be prominently displayed in clear, conspicuous 14-point bold type as a part of any informational or education materials, as well as in plan or policy documents provided to enrollees.
- The guidance outlines the very limited circumstances where insurers that have obtained a waiver can continue to sell new mini-med plans. For example, an employer that already offers a mini-med policy with a waiver may buy a new mini-med plan from a different insurer under certain circumstances. The bulletin also allows mini-med policies to be sold in States operating programs that provide health insurance coverage with low annual limits or require issuers to offer coverage with low annual limits, where either the State or the insurer has a waiver.
Other important features of the Affordable Care Act will make the health care system transparent and ensure consumers get a better value for their premium dollars. In 2011, insurance plans will be required to spend at least 80 percent of the premiums they collect from consumers on medical care, rather than on executive salaries and administrative costs. If they don’t, they will be required to provide a rebate to their customers and the percent an insurance company spends on health care must be disclosed to the public. Up to 9 million Americans could be eligible for rebates starting in 2012 that are worth up to $1.4 billion. Average rebates per person could total $164 in the individual market.
The law also requires insurance companies to publicly justify any unreasonable premium increases by publishing the justification on their websites and provides states with $250 million to strengthen their efforts to review proposed premium increases.
And the law implements landmark consumer protections that end the worst insurance company abuses. Under the new law:
- Insurers will be prohibited from denying coverage to children with pre-existing conditions, which will allow up to 72,000 uninsured children to gain coverage. Additionally, up to 90,000 children will no longer have specific benefits denied because of a pre-existing condition.
- Approximately 10,700 people whose coverage is dropped each year because they get sick and made an unintentional mistake on their application will not have their coverage rescinded.
- Before reform, cancer patients and individuals suffering from other serious and chronic diseases were too often forced to limit or go without treatment because of an insurer’s lifetime limit on their coverage. Insurance companies are now banned from placing lifetime limits on coverage. Up to 20,400 people who typically hit their lifetime limits along with nearly 102 million enrollees in plans with lifetime limits can live with the security of knowing that their coverage will be there when they need it most.
- Restrictive annual limits will be banned until all annual limits are prohibited in 2014. The ban on the use of low annual limits will protect care for up to 3,500 people each year who would have hit their annual limit. 18 million people are in plans with annual limits today.
- New insurance plans cannot charge more in cost sharing for emergency services obtained outside of their network. Up to 88 million people will benefit from this new rule.
- Up to 88 million people who enroll in new plans will be guaranteed their choice of any available primary care and pediatric doctor in their plan’s network of providers and women will have the right to see an OB/GYN without having to obtain a referral first.
- Consumers in new insurance plans will have the right to appeal decisions made by their insurance company to an independent third party.
To ensure consumers know their rights, the Administration has launched HealthCare.gov and supported state efforts to inform and protect consumers. New Consumer Assistance Program grants funded by the law will help make sure that consumers receive their new rights and benefits under the Affordable Care Act by providing grant money to States to educate consumers about their health coverage options and new programs, empower consumers to avail themselves of new protections, ensure consumers have access to accurate information, and help consumers navigate the system to find the most affordable and secure coverage that meets their needs.
For more information, read the press release about the new annual limit waiver consumer notice guidance, or you can find the guidance here
For more information on how the Affordable Care Act is creating a transparent market for health insurance, visit: http://www.healthcare.gov/news/factsheets/2010/12/increasing-transparency.html
###
* The above information is adapted from materials provided by USA Department of Health and Human Services (HHS)
** More information at USA Department of Health and Human Services (HHS)




















