Anti-Depressants Boost Brain Cells after Injury in Early Studies
Anti-Depressants Boost Brain Cells after Injury in Early Studies
Observation in Patients Leads Neurosurgeon to Take a Closer Look
Anti-depressants may help spur the creation and survival of new brain cells after brain injury, according to a study by neurosurgeons at the University of Rochester Medical Center.
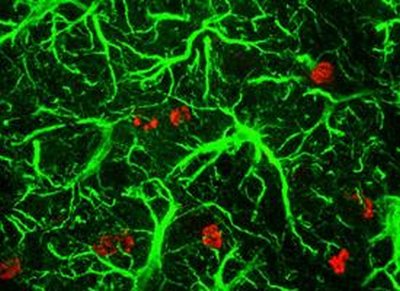
- New astrocytes generated in the hippocampus after treatment with imipramine.
Jason Huang, M.D., and colleagues undertook the study after noticing that patients with brain injuries who had been prescribed anti-depressants were doing better in unexpected ways than their counterparts who were not taking such medications. Not only did their depression ease; their memory also seemed improved compared to patients not on the medication.

“We saw these patients improving in multiple ways – their depression was improved, but so were their memory and cognitive functioning. We wanted to look at the issue more, so we went back to the laboratory to investigate it further,” said Huang, associate professor of Neurosurgery and chief of Neurosurgery at Highland Hospital, an affiliate of the University of Rochester Medical Center.
The team’s findings were published online recently in the Journal of Neurotrauma.
Huang said many patients who have a traumatic brain injury also experience depression – by some estimates, half of such patients are depressed. Doctors aren’t sure whether the depression is a byproduct of the sudden, unfortunate change in circumstances that patients find themselves in, or whether the depression is a direct consequence of brain damage.
Previous research by other groups indicated that anti-depressants help generate new brain cells and keep them healthy in healthy animals. That, together with the experience of his patients, led Huang to study the effects of the anti-depressant imipramine (also known as Tofranil) on mice that had injuries to their brains.
Scientists found that imipramine boosted the number of neurons in the hippocampus, the part of the brain primarily responsible for memory. By one measure, mice treated with imipramine had approximately 70 percent more neurons after four weeks than mice that did not receive the medication.
That change was borne out on behavioral tests as well. The team tested mice by using what scientists call a novel object recognition test. Like human infants, mice tend to spend more time sizing up objects that they haven’t encountered before – or don’t remember encountering – than they do objects that they’ve seen before. This gives scientists a way to measure a mouse’s memory.
The team found that mice that had been treated with imipramine had a better memory. They were more likely to remember objects they had seen previously and so spent more time exploring truly novel objects, compared to mice that did not receive the compound.
The benefits did not extend to the motor skills of the mice – a finding that parallels what neurosurgeons like Huang have seen in their patients on anti-depressants, who don’t show improved mobility after use of the medications.
Scientists aren’t sure whether the drug helps spur the creation of more new neurons, or whether it helps newly created neurons survive – or both. Some of the team’s evidence indicates that the drug helps immature stems evolve into useful cells such as neurons and astrocytes, and to travel to the exact areas of the brain where they’re needed.
In addition to sorting out those questions, investigators will try to identify the molecular pathway that prompts the brain to create more neurons in response to anti-depressants. The team suspects that a molecule known as BDNF or brain-derived neurotrophic factor may play a role.
Huang notes that one of his mentors, co-author Douglas H. Smith, M.D., of the University of Pennsylvania, has found that a brain injury itself also seems to prompt the brain to create more brain cells, perhaps as a way to compensate for injury.
“The brain has an intrinsic mechanism to repair itself to a certain extent,” said Huang. “Our goal is to learn more about that mechanism and improve it, to help patients recover even more brain function than they can now, even with extensive work and rehabilitation.”
Some of Huang’s work is based on his experiences treating soldiers and civilians while working for four months as a neurosurgeon with the U.S. Army Reserve in Iraq, as well as more than a decade of experience treating patients affected by incidents like motor vehicle accidents.
He said that traumatic brain injury – an injury experienced by approximately 1.4 million Americans each year – must be treated aggressively. Often this involves surgery to relieve pressure on the brain, other procedures to protect the brain against immediate further injury, and then rehabilitation for months or years.
“It’s exciting that the study involves a drug that is already safe and approved by FDA and is used clinically. If we could add a medication to the treatment regimen – even a slight improvement would be a big gain for these patients. It’s our hope that the work will ultimately make a difference in patient care,” added Huang, who is also a scientist in the Center for Neural Development and Disease.
In addition to Huang, other authors at Rochester include post-doctoral associates Xiaodi Han, M.D., Ph.D., Jing Tong, M.D., and Jiankai Yang, M.D.; neurosurgery resident Arash Farahvar, M.D.,; and undergraduate Ernest Wang. Other authors include Jun Zhang, M.D., of the Chinese PLA General Hospital in Beijing; Uzma Samadani, M.D., Ph.D., of New York University; and Douglas H. Smith, M.D., of the University of Pennsylvania.
The work was funded by the National Institute of Neurological Disorders and Stroke and by the University of Rochester.
* The above story is reprinted from materials provided by University of Rochester Medical Center



















