Individual differences in anthrax susceptibility discovered by scientists
Individual differences in anthrax susceptibility discovered by scientists
Susceptibility to anthrax toxin is a heritable genetic trait that may vary tremendously among individuals, according to a new study by researchers at the Stanford University School of Medicine.
Among 234 people studied, the cells of three people were virtually insensitive to the toxin, while the cells of some people were hundreds of times more sensitive than those of others. The findings may have important implications for national security, as people known to be more resistant to anthrax exposure could be effective first-line responders in times of crises.
The research also highlights the fact that many lethal pathogens, including HIV, malaria, leprosy and hepatitis, rely on interactions with host genes to infect and replicate within human cells. Inherited differences in the level of expression of these genes can lead to large variations in the relative susceptibility of different individuals to the pathogen.
The research was published online Feb. 6 in the Proceedings of the National Academy of Sciences. The senior author of the report is professor of genetics Stanley N. Cohen, MD, the Kwoh-Ting Li Professor at the School of Medicine. Postdoctoral scholar Mikhail Martchenko, PhD, is the first author. Collaborating in analysis of the data were associate professor of genetics Hua Tang, PhD, and research associate Sophie Candille, PhD. The study was funded by the Defense Threat Reduction Agency of the U.S. Department of Defense.
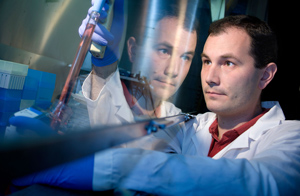
Mikhail Martchenko is the first author of a study that showed great variability in the way that cells from different people respond to the anthrax toxin.
“Every pathogen has its own virulence strategy,” said Stanford professor of microbiology and immunology and of medicine David Relman, MD, the chair of the Institute of Medicine’s Forum on Microbial Threats and a member of the U.S. Department of Health and Human Service’s National Science Advisory Board for Biosecurity, who was not involved in the research. “We already knew that infection by the same organisms in different people can have different outcomes. But until now it’s been very difficult to determine whether this variability was due to genetic or environmental factors. This is one of the few studies that has successfully identified a host-genetics-based molecular cause of this variability.”
Relman is also the chief of infectious diseases at the Veterans Affairs Palo Alto Health Care System, and the president-elect of the Infectious Diseases Society of America. In addition, he was the vice chair of the National Academy of Sciences’ committee charged in 2008 with reviewing the scientific approaches used in the FBI investigation of the anthrax attacks of 2001.
“This paper is an important contribution to our understanding of the mechanisms of host susceptibility to anthrax,” said Alan Rudolph, PhD, the director of the Chemical and Biological Technologies Directorate at the Defense Threat Reduction Agency. “We are committed to supporting outstanding science in this field and will seek opportunities to translate key discoveries such as this into useful applications in diagnostics and medical countermeasures for enhanced preparedness for the department of defense and global health security.”
In the new study, Cohen and his colleagues found that variation in the level of expression of a gene that produces a cell-surface protein called CMG2 affects the success of the anthrax toxin in gaining entry into human cells. The research suggests that analogous effects may occur in people exposed to anthrax bacteria. The authors suggest that the investigational approach they used may be broadly applicable for learning about individual susceptibility to various pathogens in human populations.
Cohen’s laboratory has been studying host gene exploitation by pathogens for several years; they’ve termed such genes “cellular genes exploited by pathogens,” or CGEPs. They’ve identified and categorized CGEPs in an electronic registry. This registry makes it easier to identify correlations between variations in particular genes and a pathogen’s virulence. Rather than searching blindly through the genomes of many individuals (an approach known as a genome wide association study) for associations, the researchers can instead home in on and look for variations in the much smaller number of host genes already known to play a role in infection. The registry also provides possible targets for drugs designed to prevent or treat infection by disrupting the exploitation of host genes by pathogens.
Anthrax disease is caused by infection with the anthrax bacteria. Spores of the bacteria exist naturally in the environment. When inhaled by humans or animals (commonly livestock), the spores are transported by immune cells to lymph nodes, where the bacteria begin to multiply and are secreted into the bloodstream. Once in the bloodstream, the bacteria begin to produce the anthrax toxin that infiltrates and kills host cells. Untreated, anthrax infection can cause widespread tissue damage, bleeding and death.
Previous studies had shown that CMG2 is the principal cell-surface protein bound by an anthrax toxin component called “protective antigen.” This binding allows protective antigen to smuggle into the host cell two other toxin proteins that then kill the cell. Cohen and Martchenko wondered whether naturally occurring variations in either the sequence or the levels of expression of CMG2 would affect the killing ability of the toxins.
To find out, the researchers used cells obtainable through the International HapMap Project — an effort to catalog and understand genetic diversity in human populations. The researchers studied immune cells called lymphocytes collected from 234 individuals of varying ethnic and geographic backgrounds: 84 Nigerians, 63 Americans whose ancestors came from northern and western Europe, 44 Japanese and 43 Han Chinese.
They found that, of the 234 samples, lymphocytes from three individuals of European ancestry were thousands of times more resistant to killing by an engineered hybrid toxin brought into the cells by protective antigen. (The researchers couldn’t use the natural anthrax toxin because it doesn’t kill lymphocytes — one of the few cell types available through the HapMap project.)
The extent of variation in sensitivity was surprising to the scientists. Even excluding the virtually resistant cells, they sometimes had to apply as much as 250 times more toxin to kill a similar number of cells in one sample as in another. In addition, they observed that cells isolated from parents and their children responded similarly, indicating that toxin sensitivity is an inherited trait.
The researchers next modified mouse cells to express varying levels of human CMG2 on their surface. They found a direct correlation between the level of expression of CMG2 and the ability of toxin to kill the cells: increased expression of CMG2 resulted in increased toxin sensitivity, possibly by providing more entry points for the toxin.
Finally, the researchers also examined whether there was any correlation between a common sequence variation in the CMG2 gene and anthrax susceptibility. They found that creating a similar sequence variation altered the susceptibility of mouse cells to toxin. However, the correlation of this change with toxicity was not statistically significant in the human lymphocyte populations they studied.
“This research offers an important proof of principle,” said Relman. “They’ve showed that genetically-determined variations in the level of expression of a human protein can influence the susceptibility of host cells to anthrax toxin. The findings also provide a possible means for predicting who is likely to become seriously ill after exposure, which could be extremely useful when faced with a large number of exposed people, such as was the case during the 2001 anthrax attacks. Finally, they could lead to the development of novel treatment strategies, perhaps by blocking the interaction between the toxin and the receptor, or by down-regulating its expression.”
The authors note in the study that the research has implications beyond anthrax exposure. “Our findings, which reveal the previously unsuspected magnitude of genetically determined differences in toxin sensitivity among cells from different individuals, suggest a broadly applicable approach for investigating pathogen susceptibility in diverse human populations.”
Information about Stanford’s Department of Genetics, in which the research was conducted, is available at http://genetics.stanford.edu/.
BY KRISTA CONGER
Stanford University Medical Center
Photo of Martchenko by Steve Fisch
###
* Stanford University Medical Center integrates research, medical education and patient care at its three institutions – Stanford University School of Medicine, Stanford Hospital & Clinics and Lucile Packard Children’s Hospital.
** The above story is adapted from materials provided by Stanford University School of Medicine
________________________________________________________________




















