Improved COPD Detection
Improved COPD Detection
A new technique can distinguish between different types of chronic obstructive pulmonary disease (COPD) and track disease progression. The method could allow for more accurate diagnoses and lead to more effective treatments for COPD.
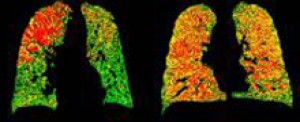
PRM images can help distinguish healthy lung areas (green) from those with early-stage damage (yellow) and emphysema (red). Image courtesy of University of Michigan Center for Molecular Imaging.
COPD is a lung disease that makes it hard to breathe. In people who have COPD, airway tubes to the lungs narrow, making it hard to get air in and out. COPD can cause wheezing, shortness of breath, chest tightness and coughing that produces large amounts of mucus. Cigarette smoking is the leading cause of COPD in the United States, but the disease can have other roots as well.
COPD can involve damage to the small airways of the lungs (functional small airways disease) as well as destruction of lung tissue (emphysema). The ability to diagnose the extent of lung damage could help doctors track disease progression and personalize COPD treatments. Current CT scan methods can assess the extent of emphysema, but measuring functional small airways disease has remained a challenge.
Researchers at the University of Michigan led by Dr. Brian D. Ross set out to address the problem by adapting an image analysis technique called parametric response mapping (PRM) that they’d first developed to track tumors. In PRM, a computer matches voxels—the smallest measureable unit of volume in an image data set—between CT scans. Voxels in scans taken during a full inhalation are matched with equivalent voxels in scans taken during a full exhalation. The density of healthy lung tissue changes more between the 2 states than the density of diseased lung tissue. By comparing densities in each voxel pair, a computer program can create 3-D maps of damage throughout the entire lung.
The scientists analyzed whole-lung CT scans of 194 people with COPD acquired at both full inhalation and full exhalation in the COPDGene study, which is funded by NIH’s National Heart, Lung and Blood Institute (NHLBI). Additional funding was provided by NIH’s National Cancer Institute (NCI) and National Institute of Biomedical Imaging and Bioengineering (NIBIB). Results appeared online on October 7, 2012, in Nature Medicine.
The researchers showed that PRM could successfully identify the extent of both functional small airways disease and emphysema. They also observed a pattern in the data suggesting that functional small airways disease may precede emphysema in the progression of COPD.
To investigate whether PRM could be used to track disease progression, the researchers analyzed images from people who had undergone inspiratory/expiratory CT scanning over a period of time. They found that PRM could be used to monitor COPD progression.
“Essentially, with the PRM technique, we’ve been able to tell sub-types of COPD apart, distinguishing functional small airway disease from emphysema and normal lung function,” Ross says. “We believe this offers a new path to more precise diagnosis and treatment planning and a useful tool for precisely assessing the impact of new medications and other treatments.”
By Harrison Wein, Ph.D.
###
* The above story is reprinted from materials provided by National Institutes of Health (NIH)
** The National Institutes of Health (NIH) , a part of the U.S. Department of Health and Human Services, is the nation’s medical research agency—making important discoveries that improve health and save lives. The National Institutes of Health is made up of 27 different components called Institutes and Centers. Each has its own specific research agenda. All but three of these components receive their funding directly from Congress, and administrate their own budgets.




















