Protein Linked to Atopic Dermatitis
Protein Linked to Atopic Dermatitis
A study in mice suggests that lack of a certain protein may trigger atopic dermatitis, the most common type of eczema. The finding may lead to improved treatment options for people.
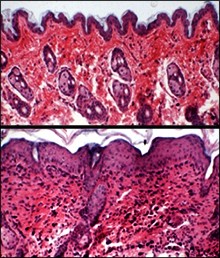
Normal skin from a mouse (top) shows no sign of inflammation. Skin from a mouse lacking Ctip2 (bottom) is heavily inflamed with eczema. Photo courtesy of Oregon State University.
Atopic dermatitis is a chronic disease in which the skin becomes itchy and inflamed. The disease can be difficult to treat. It affects an estimated 10-20% of children and 1-3% of adults nationwide. Most people outgrow atopic dermatitis by early adulthood, but for some, the disease persists. Both genes and environmental factors play a role in atopic dermatitis, but its root causes aren’t known.
Scientists believe that atopic dermatitis involves a defective skin barrier that allows allergens to enter the skin and interact with immune cells to cause inflammation. Several proteins have been identified that may be involved in this response. One is thymic stromal lymphopoietin (TSLP), which has also been linked to asthma and to a food allergy-related disorder called eosinophilic esophagitis. TSLP expression is elevated in mice with atopic dermatitis. The factors involved in this regulation, however, aren’t well understood.
Past work led by Dr. Arup Indra at Oregon State University showed that COUP-TF interacting protein 2 (Ctip2) is crucial for forming and maintaining the skin barrier in developing mouse embryos. Ctip2 was also found to be important for skin lipid metabolism, which keeps the skin healthy and hydrated.
In the new study, Indra’s team set out to explore the role of Ctip2 in the skin of adult mice. The team genetically altered mice to remove Ctip2 from epidermal (outer layer) skin cells. The study was partly funded by NIH’s National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and National Institute of Environmental Health Sciences (NIEHS). Results appeared in the December 20, 2012, issue of the online journalPLoS One.
The researchers found that around 8 to 10 weeks after birth, 67% of the mice lacking Ctip2 had dry and scaly skin and 17% also developed skin lesions. By 4 months, 89% of the altered mice displayed symptoms. Normal mice didn’t have skin issues at any age.
The team identified an age-dependent increase in certain inflammatory cells in the skin of the mice lacking Ctip2. Ctip2 deficiency also caused systemic inflammatory responses. The altered mice had enlarged lymph nodes and spleens, as well as high levels of circulating inflammatory proteins.
Expression of genes known to be involved in mouse and human atopic dermatitis, including TSLP, increased in mouse skin when Ctip2 was absent. TSLP levels were up to 1,000-fold higher. The team found evidence that Ctip2 directly regulates TSLP. Future research will be needed to determine precisely how repression of TSLP by Ctip2 might protect against disease.
“With a better understanding of just what is causing eczema on a genetic basis, we should be able to personalize treatments, determine exactly what each person needs, and develop new therapies,” Indra says. “This might be with topical compounds that increase Ctip2 expression in skin cells, or customized treatments to restore an individual person’s lipid profile.”
By Miranda Hanson, Ph.D.
###
* The above story is reprinted from materials provided by National Institutes of Health (NIH)
** The National Institutes of Health (NIH) , a part of the U.S. Department of Health and Human Services, is the nation’s medical research agency—making important discoveries that improve health and save lives. The National Institutes of Health is made up of 27 different components called Institutes and Centers. Each has its own specific research agenda. All but three of these components receive their funding directly from Congress, and administrate their own budgets.




















