Nature-Inspired Surgical Glue Mends Hearts
Nature-Inspired Surgical Glue Mends Hearts
Researchers developed a new tissue adhesive that is biodegradable, biocompatible, and easily manipulated. It could allow for less invasive surgeries that don’t require sutures or staples.
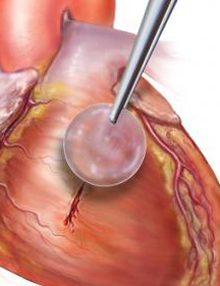
The waterproof, light-activated glue can successfully secure biodegradable patches to seal holes in a beating heart. Image courtesy of Karp Laboratory.
During surgery, reconnecting tissues and attaching prosthetic materials can be a challenge. Suturing can be time-consuming, and staples can damage tissue. Surgical adhesives could solve these problems, but current options have limitations with strength, adhesion, and toxicity. Procedures performed on delicate tissues, such as in young infants, or on tissues that are moving, such as the heart, pose particular challenges. In addition, an ideal surgical adhesive would need to be water insoluble, as flowing blood would wash away a water-soluble compound.
Inspired by the footpad of insects and the thick, sticky secretions of slugs and sandcastle worms, whose fluids can create bonds underwater, a research team led by Dr. Jeffrey Karp of Brigham and Women’s Hospital and Dr. Pedro del Nido of Boston Children’s Hospital set out to develop a similar gel-like material that could function as a stable, water-insoluble and elastic surgical glue. The work was funded in part by NIH’s National Heart, Lung, and Blood Institute (NHLBI), National Institute of General Medical Sciences (NIGMS), and National Institute of Dental and Craniofacial Research (NIDCR). The findings appeared online January 8, 2014, in Science Translational Medicine.
As their base, the scientists used a compound called poly(glycerol sebacate acrylate) (PGSA). PGSA is composed of glycerol, a basic building block of lipids, and sebacic acid, a naturally occurring fatty acid. When mixed with a special light-sensitive chemical, the resulting gel solidified upon a brief, 5-second exposure to ultraviolet (UV) light.
The researchers found that the gel easily spread over a surface and adhered to tissues in wet conditions. When exposed to UV light, it “cured” to form an adhesive that was soft, elastic, and water-tight.
The researchers extensively tested the glue in several settings. They found it had mechanical properties similar to arteries and the digestive tract. Patches coated with the glue stayed attached to the quickly beating hearts of rats without altering heart function. The scientists also successfully used the glue to seal a defect in the wall of a rat heart.
The team next tested the glue in pigs, which have a heart rate similar to that of humans. They attached patches inside beating hearts and showed that the patches remained in place when heart rate and blood pressure increased. Using the glue alone, they were able to create a leak-proof seal in the carotid artery of pigs.
“This adhesive platform addresses all of the drawbacks of previous systems in that it works in the presence of blood and moving structures,” del Nido says. “It should provide the physician with a completely new, much simpler technology and a new paradigm for tissue reconstruction to improve the quality of life of patients following surgical procedures.”
The technology has been licensed to a company, and patents based on the study have been filed. However, long-term experiments will be needed to further evaluate the gel before it can be tested in people.
By Carol Torgan, Ph.D.![]()
###
* The above story is reprinted from materials provided by National Institutes of Health (NIH)
** The National Institutes of Health (NIH) , a part of the U.S. Department of Health and Human Services, is the nation’s medical research agency—making important discoveries that improve health and save lives. The National Institutes of Health is made up of 27 different components called Institutes and Centers. Each has its own specific research agenda. All but three of these components receive their funding directly from Congress, and administrate their own budgets.




















