HHS to increase efforts to create savings for states; ensure sustainability and quality in Medicaid program
Sebelius outlines state flexibility and federal support available for Medicaid
HHS to increase efforts to create savings for states; ensure sustainability and quality in Medicaid program
Sebelius outlines state flexibility and federal support available for Medicaid
HHS to increase efforts to create savings for states; ensure sustainability and quality in Medicaid program
WASHINGTON – Today, HHS Secretary Kathleen Sebelius sent a letter to governors outlining the flexibility and support available to states that are examining how to make Medicaid programs more efficient while meeting pressing health care challenges in the face of difficult budget circumstances.
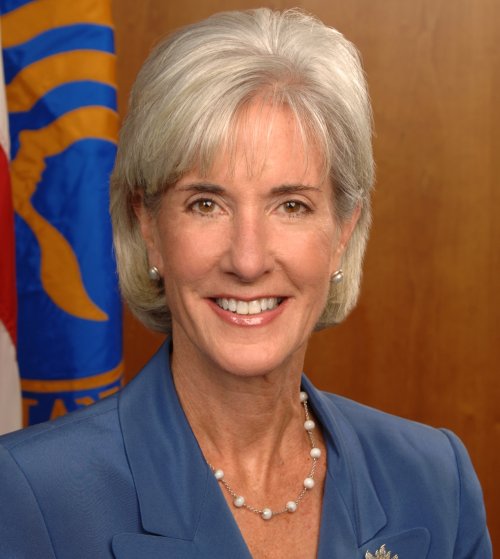
“In light of difficult budget circumstances, we are stepping up our efforts to help you identify cost drivers in the Medicaid program and provide you with new tools and resources to achieve both short-term savings and longer-term sustainability while providing high-quality care to the citizens of your states,” Sebelius wrote in the letter. “We are committed to responsiveness and flexibility, and will expedite review of state ideas.”
Over the past two years, the administration has worked to provide additional support for states to manage their Medicaid program by working with Congress to increase federal support for the states through an enhanced federal match for Medicaid (known as the Federal Medical Assistance Percentage or FMAP), and, at the request of many governors, extending the enhanced FMAP policy through June 2011. In 2009 alone, due to the enhanced FMAP, state Medicaid spending fell by ten percent even though enrollment in Medicaid climbed by seven percent due to the recession.
In addition to this financial support, the administration has taken administrative steps to open up lines of communication with states, lower the paperwork burden states face in administering the program, and accelerate the review process for state plan amendments.
The letter also outlines the substantial flexibility that states have to design benefits, service delivery systems, and payment strategies, without a waiver. In 2008, roughly 40 percent of Medicaid benefits spending, $100 billion, was spent on optional benefits for all enrollees, with nearly 60 percent of this spending for long-term care services. In addition, the letter describes new initiatives that HHS will pursue with states, and offers state-specific technical support.
Some of the key areas of potential cost savings include:
– Changing Benefits. States can generally change optional benefits or limit their amount, duration or scope through an amendment to their state plan. In addition, states may add or increase cost sharing for services within limits.
– Managing Care for High-Cost Enrollees More Effectively. Just 5 percent of Medicaid beneficiaries account for more than half of all of Medicaid’s costs. These individuals often have fragmented care that contributes to higher costs. A new option to provide “health homes” to people with chronic illnesses, and initiatives to reduce unnecessary hospital readmissions, are just some of the strategies that can help improve care and lower costs.
– Purchasing Drugs More Efficiently. States have broad flexibility to set their pharmacy pricing. HHS will create a first-ever national database of actual acquisition costs that states can use to determine state-specific rates. HHS will also share proven approaches that states have used to drive down costs.
– Assuring Program Integrity. States will be able to use federal audit contractors to save funds and consolidate auditing efforts and will benefit from new, cutting-edge analytics, like predictive modeling, being developed to prevent fraud in the Medicare program. HHS’ Medicaid Integrity Institute is preparing a series of webinars for states to share best practices for assuring program integrity.
The full letter…
Sebelius outlines state flexibility and federal support available for Medicaid – (Full Letter) February 3, 2011
Dear Governor:
As the new year begins, officials at the Federal and State level are looking ahead to a period full of opportunities and challenges. I have had the opportunity to speak individually with many of you over the past few weeks, including many who are now assuming their new positions. Having served as a Governor, let me welcome you to one of the best jobs you will ever have.
In these conversations, I have heard the urgency of your State budget concerns. I know you are struggling to balance your budget while still providing critical health care services to those who need them most. I want to reaffirm the Obama Administration’s commitment to helping you do both.
I also know that as you prepare your budget, your attention will turn to Medicaid. Medicaid is a major source of coverage for children, pregnant women, seniors and people with disabilities in every State. It has a unique role in our health care system, covering a diverse group of beneficiaries, including some of the most frail and vulnerable Americans. And it is the nation’s primary payer for long-term care in nursing homes and outside of institutions. Medicaid is a Federal-State health partnership. The Federal government pays a fixed percentage or matching rate and sets minimum standards. States fund their share of program costs and have the lead on designing their programs beyond these standards, including what benefits are covered, how providers are paid, and how care is delivered.
In the last two years, the Administration has worked to ensure adequate support for States to manage their Medicaid and the Children’s Health Insurance Programs (CHIP). One of the first actions taken by President Obama was to work with Congress on legislation to increase Federal support for the States in the form of an enhanced Federal match for Medicaid (known as the Federal Medical Assistance Percentage or FMAP). This enhanced FMAP was part of the American Recovery and Reinvestment Act and lasted through December 31, 2010. However, last year, at the request of many Governors, we worked with Congress to extend the enhanced FMAP policy through June 2011. Approximately $100 billion has been provided to States, and in 2009 alone, due to the enhanced FMAP, State Medicaid spending fell by ten percent even though enrollment in Medicaid climbed by seven percent due to the recession. In addition to this financial support, we have taken many other administrative steps to open up lines of communication with States, lower the paperwork burden States face in administering the program, and accelerate our review process for State plan amendments.
We recognize that many States are re-examining their Medicaid programs and looking for opportunities to meet the pressing health care challenges and better cope with rising costs. In light of difficult budget circumstances, we are stepping up our efforts to help you identify cost drivers in the Medicaid program and provide you with new tools and resources to achieve both short-term savings and longer-term sustainability while providing high-quality care to the citizens of your States. We are committed to responsiveness and flexibility, and will expedite review of State proposals.
Starting immediately, the senior leadership from across the Department will be available to meet individually with your staff about plans that you may already have in mind. My team stands ready to come to your State to discuss your priorities and how we can help achieve them.
In the meantime, recent conversations suggest a lack of clarity about what flexibility currently exists in Medicaid. Some of you have asked whether I can “waive” the maintenance of effort requirements for people who a State has covered under Medicaid’s “optional” eligibility categories and waivers. I note that the Affordable Care Act gives a State the flexibility to reduce eligibility for non-disabled, non-pregnant adults with incomes above 133 percent of the Federal poverty line ($14,500 for an individual) if the State has a budget deficit, although prior to June 30, this would mean the loss of the enhanced FMAP under the Recovery Act. I continue to review what authority, if any, I have to waive the maintenance of effort under current law.
However, States have substantial flexibility to design benefits, service delivery systems, and payment strategies, without a waiver. In 2008, roughly 40 percent of Medicaid benefits spending – $100 billion – was spent on optional benefits for all enrollees, with nearly 60 percent of this spending for long-term care services. The enclosed paper identifies a range of State options and opportunities to more efficiently manage Medicaid, many of which are underway across the country. Some of the key areas of potential cost savings are described briefly below:
– Modifying Benefits. While some benefits, such as hospital and physician services, are required to be provided by State Medicaid programs, many services, such as prescription drugs, dental services, and speech therapy, are optional. States can generally change optional benefits or limit their amount, duration or scope through an amendment to their State plan, provided that each service remains sufficient to reasonably achieve its purpose. In addition, States may add or increase cost sharing for services within limits (see attachment for details). Some States have opted for more basic benefit packages for higher-income enrollees (e.g., Wisconsin provides benefits equivalent to the largest commercial plan offered in the State plus mental health and substance disorder coverage for pregnant women with income between 200 and 250 percent of poverty). A number of States charge beneficiaries $20 for non-urgent emergency room visits or use cost sharing for prescription drugs to steer individuals toward generics or preferred brand-name drugs. To the extent States scale back low-value benefits or add fair cost sharing that lowers inappropriate use of care, savings can be generated.
– Managing Care for High-Cost Enrollees More Effectively. Just one percent of all Medicaid beneficiaries account for 25 percent of all expenditures. Initiatives that integrate acute and long-term care, strengthen systems for providing long-term care to people in the community, provide better primary and preventive care for children with significant health care needs, and lower the incidence of low-birth weight babies are among the ways that States have improved care and lowered costs. For example, children’s hospitals adopting a medical home model to manage the care of chronically ill children have accomplished impressive improvements in health and reductions in cost. One Florida children’s hospital reduced emergency room visits by more than one-third, and reduced hospital days by 20 percent. These delivery models and payment strategies can be implemented by hospitals and States without seeking a Federal waiver, and we are exploring ways that we might provide further support for such initiatives.
In addition, the Affordable Care Act offers new Medicaid options that provide States with additional Federal matching funds. For example, States can now benefit from a 90 percent Federal matching rate for coordination of care services provided in the context of a health home for people with chronic conditions. Additionally, the Community First Choice Option, available in October, will offer States a six percent increase in the Federal matching rate to provide certain person-centered long-term care services and supports to enhance your efforts to serve beneficiaries in community-based settings.
– Purchasing Drugs More Efficiently. In 2009, States spent $7 billion to help Medicaid beneficiaries afford prescription drugs. States have broad flexibility to set their pharmacy pricing. We are committed to working with States to ensure they have accurate information about drug costs in order to make prudent purchasing decisions. As recommended by States, the Department is undertaking a first-ever national survey to create a database of actual acquisition costs that States may use as a basis for determining State-specific rates, with results available later this year. Alabama, the first State to adopt use of actual acquisition costs as the benchmark for drug reimbursement, expects to save six percent ($30 million) of its pharmacy costs in the first year of implementation. We will also share additional approaches that States have used to drive down costs, such as relying more on generic drugs, mail order, management relating to over-prescribed high cost drugs, and use of health information technology to encourage appropriate prescribing and avoidance of expensive adverse events.
– Assuring Program Integrity. According to the Department’s 2010 Financial Agency Report, the three-year weighted average national error rate for Medicaid is 9.4 percent, meaning that $33.7 billion in combined Federal and State funds were paid inappropriately. The Federal government and States have a strong, shared interest in assuring integrity in every aspect of the program, and there are new options and tools available to States. Our Medicaid Integrity Institute is preparing a series of webinars for States to share best practices, learn about the potential cost savings created by the new program integrity provisions in the Affordable Care Act, and hear about initiatives underway in Medicare and the private sector that could be replicated in Medicaid. For example, to help your State identify providers who were terminated elsewhere, States will have access to a new Federal portal starting in mid-February to obtain this information from other States and the Medicare program. In addition, States will be able to use Federal audit contractors to save State funds and consolidate auditing efforts. States will also benefit from new, cutting-edge analytics, like predictive modeling, being developed to prevent fraud in the Medicare program. In 2010, the Departments of Health and Human Services and Justice recovered more than $4 billion in taxpayer dollars – the highest annual amount ever – from people who attempted to defraud seniors and taxpayers, and we want to continue to work closely with you to prevent and fight waste, fraud and abuse in Medicare, Medicaid and CHIP. The President is committed to cutting the error rate in half by 2012.
Beyond these areas of flexibility that could produce short-term savings, we are actively moving forward in areas that could lower costs in the long run. In particular, we are focused on how to help States provide better care and lower costs for so called “dual eligibles,” seniors and people with disabilities who are eligible for both Medicaid and Medicare. These individuals represent 15 percent of Medicaid beneficiaries but nearly 40 percent of all Medicaid spending. This population offers great potential for improving care and lowering costs by replacing the fragmented care that is now provided to these individuals with integrated care delivery models. The new Federal Coordinated Health Care Office has already released a solicitation for up to 15 States to receive Federal support to design new models for serving dual eligibles. We also plan to launch a Department-wide effort to reduce the costs of health care by improving patient safety in Medicare, Medicaid and throughout the private health care system, and States will be critical partners in this effort. We welcome other ideas on new models of care, including new ways to deliver care that encourage investment and yield savings.
To expedite these 2011 efforts, we will host a series of “virtual” meetings with State health policy advisors and Medicaid directors. In these sessions, we will share information about promising Medicaid cost-saving initiatives underway in one or more States that we are prepared to support and approve in other States on a fast-track basis.
This is just the beginning of a discussion on how we can help you better manage your Medicaid programs and navigate your budget crises. Please be assured that I am committed to working with you toward a sustainable and vibrant Medicaid system in ways that are responsive to the current challenges you are facing every day.
Sincerely,
/s/
Kathleen Sebelius
Enclosures: http://medicinezine.com/information/medicaid-cost-savings-opportunities/
* The above story is reprinted from materials provided by USA Department of Health and Human Services (HHS)
** More information at USA Department of Health and Human Services (HHS)




















