New Vasculitis Therapy as Effective as Standard Care
New Vasculitis Therapy as Effective as Standard Care
Patients with severe vasculitis, or inflammation of the blood vessels, get the same benefits from just 4 doses of the drug rituximab over a month as from the standard daily therapy for 18 months, a new study reports.
Vasculitis arises when your immune system mistakenly attacks your blood vessels. What causes this attack isn’t fully known, but it can result from infection or certain medications.
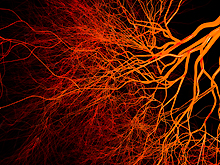
Severe forms of vasculitis can be caused by the rare autoimmune diseases microscopic polyangiitis and granulomatosis with polyangiitis. People with these conditions produce harmful antibodies (anti-neutrophil cytoplasmic antibodies, or ANCAs) that attack immune cells known as neutrophils. Resulting inflammation in small- to medium-sized blood vessels can cause severe organ damage and sometimes death.
The current standard of care for ANCA-related vasculitis requires daily doses of the harsh immunosuppressant drug cyclophosphamide for 3 to 6 months. Daily doses of another immunosuppressant, azathioprine, then follow for a year or more. This standard therapy usually clears the vasculitis, but relapse is common. In addition, this treatment suppresses the immune system in a non-specific way and has potentially severe side effects. In contrast, the drug rituximab is specifically targeted to deplete the type of immune cells thought to produce ANCA.
A team of international researchers tested to see how rituximab compares to the standard treatment for ANCA-related vasculitis. Funded in part by NIH’s National Institute of Allergy and Infectious Diseases (NIAID), the team studied 197 vasculitis patients. Led by Dr. Ulrich Specks of the Mayo Clinic and Dr. John Stone of Massachusetts General Hospital, the scientists divided patients into 2 groups. One received 4 weekly infusions of rituximab. The other received the standard therapy. All participants received steroid treatment. Those who went into remission stopped receiving steroids after 6 months.
Short-term results, reported in 2010, found that 64% of those taking rituximab were free of disease after 6 months compared to 53% of those receiving standard care. Based on these findings, the U.S. Food and Drug Administration approved rituximab combined with steroids for treating granulomatosis with polyangiitis and microscopic polyangiitis.
The researchers followed trial participants for an additional year to evaluate rituximab’s long-term efficacy and safety. Their new findings appeared in the August 1, 2013, issue of the New England Journal of Medicine.
After 18 months, rituximab continued to be as effective as the standard regimen. There were no signs of active disease in 39% of participants who received rituximab and 33% of those who received standard care. No major differences were seen in average length of remission or in the frequency and severity of relapses. Adverse events, such as infection, occurred at similar rates in both groups.
“The data from this trial suggest that intermittent retreatment with rituximab could be a more effective approach to long-term disease control than daily immunosuppression for patients who are at a high risk for relapse,” says Specks.
###
* The above story is reprinted from materials provided by National Institutes of Health (NIH)
** The National Institutes of Health (NIH) , a part of the U.S. Department of Health and Human Services, is the nation’s medical research agency—making important discoveries that improve health and save lives. The National Institutes of Health is made up of 27 different components called Institutes and Centers. Each has its own specific research agenda. All but three of these components receive their funding directly from Congress, and administrate their own budgets.




















