More Interventions at Delivery Not Linked to Healthier Newborns
More Interventions at Delivery Not Linked to Healthier Newborns
High Rates of Induction, Primary C-Section Do Not Improve Infant Outcomes in Low-Risk Women at Community Hospitals
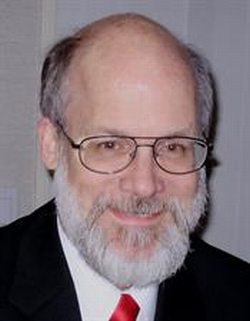
- Christopher Glantz, M.D., M.P.H.
The finding that rates of intervention at delivery – whether high, low, or in the middle – had no bearing on the health of new babies brings into question the skyrocketing number of both inductions and cesarean deliveries in the United States.
“Like virtually all medical therapies and procedures, these interventions entail some risk for the mother, and there is no evidence in this study that they benefit the baby,” said Christopher Glantz, M.D., M.P.H., study author and professor of Maternal Fetal Medicine at the University of Rochester Medical Center. “In my mind, if you are getting the same outcome with high and low rates of intervention, I say ‘Do no harm’ and go with fewer interventions.”
Similar to other fields of medicine, great variation exists in obstetric practices, particularly in rates of induction of labor and cesarean delivery. A limited number of studies have examined if and how these rates are associated with improvement in the health of newborns and reported mixed results.
“More is better’ seems to be the epitome of U.S. healthcare today, with doctors and patients often choosing to do more rather than less, even when there is no evidence to support it,” noted Glantz. “But, as our study suggests, more may not always be better.”

Glantz acknowledges that the optimal rate of any medical intervention is difficult to define, and that larger studies are needed to better understand the relationship between intervention and outcome. In the meantime, he believes it’s hard to justify high rates of interventions – especially elective – in low-risk pregnant women without any known benefits to newborns, given that these interventions pose maternal risks.
In the study, Glantz focused on pregnant women delivering in level I hospitals – those lacking a Neonatal Intensive Care Unit or NICU – because they care primarily for low-risk women who do not have major complications, such as diabetes, high blood pressure or other severe disease. The majority of women in the United States deliver in level I hospitals.
Through a birth certificate database, Glantz obtained and analyzed data from 10 level I hospitals in the Finger Lakes Region of upstate New York and calculated the rates of induction and cesarean delivery at each between 2004 and 2008. Not surprisingly, the rates varied widely.
To determine the health of newborns delivered at these hospitals, he looked at three outcomes: transfer of the newborn to a hospital with a NICU (signifying the presence of complications that required a higher level of care); immediate ventilation or breathing assistance; and a low 5-minute Apgar score (a quick assessment of the overall wellbeing of a newborn).
Using statistical models, Glantz assessed the relationship between rates of induction and cesarean delivery and rates of the three neonatal outcomes. He found intervention rates had no consistent effect on newborns: Whether a hospital did a lot or very few interventions, there was no association with how sick or healthy the infants were.
Even after a second round of analysis that accounted for differences among pregnant women that could potentially impact the results, the finding was the same – hospitals with high intervention rates had newborn outcomes indistinguishable from hospitals with low rates.
According to Glantz, “If higher intervention rates were preventing negative outcomes that otherwise would have occurred, and lower intervention rates led to negative outcomes that potentially could have been avoided, the data would have revealed these relationships, but there were no such trends.”
The study included a group of approximately 28,800 women who labored (some naturally and some induced), followed by re-analysis of 29,700 women who had no history of previous cesarean section (some of whom ultimately delivered vaginally and others by cesarean section). Many women in the first group were also analyzed in the second group. Women who had had a previous cesarean delivery were excluded from the second analysis, because more than 90 percent of women with previous cesareans deliver by repeat cesarean, and these are not necessarily being done to benefit the newborns.
Glantz recognizes that some labor inductions and cesarean sections, when done for specific, established medical reasons, are necessary and lead to improved outcomes. But some interventions are elective or marginally indicated, driven by social reasons such as convenience and patient requests to deliver with “their” physician.
Labor induction is not always successful and is associated with an increased likelihood of cesarean delivery. Cesarean delivery, while common, is a major surgery and like all surgeries increases the risk of infection, bleeding, the need for additional surgeries, and results in longer recovery times.
“It is always important to try to find out when interventions will do the most good, and this study is one more log on the fire for researchers and physicians exploring these issues,” said Jennifer Bailit, M.D., M.P.H, a maternal fetal medicine expert at the MetroHealth Medical Center in Cleveland who conducts similar research. “Understanding when and how an intervention can best improve outcomes is important to physicians and patients.”
The study was funded by the University of Rochester Medical Center and the New York State Department of Health. A major strength of the study is its large size, while limitations include the inability to assess and control for all possible factors influencing interventions – a constraint of database research.
* For Media Inquiries: Emily Boynton 585-273-1757
** The above story is reprinted from materials provided by University of Rochester Medical Center




















