Insights Into Tumor-Associated Epilepsy
Insights Into Tumor-Associated Epilepsy
Glioma, one of the most deadly and common types of brain tumor, is often associated with seizures, but the origins of these seizures and effective treatments for them have been elusive. A new study sheds light on the cause and suggests potential therapies.
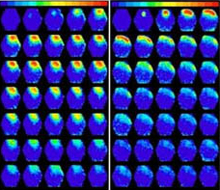
- After electrical stimulation, there is a prolonged, broader spread of activity (yellow and red areas) in mouse brain tissue containing a glioma (left) compared to normal mouse brain tissue (right). Adjacent frames are 1.8 milliseconds apart.Courtesy of Dr. Harald Sontheimer, University of Alabama Birmingham.
About 80% of people with glioma experience at least one seizure during their illness, often as the first symptom. Sen. Ted Kennedy, D-Mass., whose death was caused by a malignant glioma in August 2009, was diagnosed after having a seizure 15 months earlier. About one-third of patients develop recurring seizures, known as tumor-associated epilepsy.
Elevated levels of a brain signaling molecule called glutamate are known to cause abnormal electrical activity in the brain that can lead to epileptic seizures. Release of excess glutamate from brain cells called glia appears to play a role in some types of epilepsy. Because gliomas result from an overgrowth of glia, researchers had theorized that glutamate produced by the tumors might cause seizures, but no one had established a causal link.
A team led by Dr. Harald Sontheimer at the University of Alabama Birmingham (UAB) tested the theory by studying mice whose brains were seeded with human glioma cells. The study was funded by NIH’s National Institute of Neurological Disorders and Stroke (NINDS), including grants funded through the American Recovery and Reinvestment Act. The results appeared online on September 11, 2011, in Nature Medicine.
About one-third of the animals with gliomas developed abnormal brain activity and behavioral signs consistent with seizures. The researchers investigated how the tumors affect brain activity in response to stimulation. When they delivered electrical pulses near tumors, they found the regions to be hyperexcitable. The stimulation led to more prolonged and widespread activity in tumor-containing regions than in normal brain tissue. Brain tissue containing the tumors also released higher levels of glutamate.
The researchers tested whether sulfasalazine, a drug on the market for treating certain inflammatory disorders, could correct these abnormalities. Sulfasalazine is known to target a protein complex called the system Xc(-) transporter, which appears to be the major driver for release of glutamate from glioma cells. The team found that sulfasalazine reduced glutamate release from gliomas. The drug also reduced seizure activity in the glioma-bearing mice, cutting the frequency of epileptic bursts nearly fivefold in the first hour after treatment. The effects of the drug lasted for about 4 hours.
“People have assumed that tumors cause seizures by irritating the brain, but that really isn’t a scientific explanation. We have now shown that the seizures are caused by glutamate release from the tumor,” Sontheimer says.
Whether these promising results will directly translate into improved outcomes in patients with brain tumors remains to be tested. A small trial of people with advanced stage gliomas treated with varying doses of sulfasalazine was terminated early due to safety concerns. A clinical trial is now planned at UAB to determine if the drug can reduce seizures in people with slow-growing gliomas. Meanwhile, Sontheimer’s lab is working with medicinal chemists to develop a form of the drug that is more stable in the bloodstream and brain, and more active against system Xc(-).
* The above story is reprinted from materials provided by National Institutes of Health (NIH)
** The National Institutes of Health (NIH) , a part of the U.S. Department of Health and Human Services, is the nation’s medical research agency—making important discoveries that improve health and save lives. The National Institutes of Health is made up of 27 different components called Institutes and Centers. Each has its own specific research agenda. All but three of these components receive their funding directly from Congress, and administrate their own budgets.

















