Cancer costs projected to reach at least $158 billion in 2020
Cancer costs projected to reach at least $158 billion in 2020
New NIH study projects survivorship and costs of cancer care based on changes in the US population and cancer trends
Based on growth and aging of the U.S. population, medical expenditures for cancer in the year 2020 are projected to reach at least $158 billion (in 2010 dollars) — an increase of 27 percent over 2010, according to a National Institutes of Health analysis. If newly developed tools for cancer diagnosis, treatment, and follow-up continue to be more expensive, medical expenditures for cancer could reach as high as $207 billion, said the researchers from the National Cancer Institute (NCI), part of the NIH. The analysis appears online, Jan. 12, 2011, in the Journal of the National Cancer Institute.
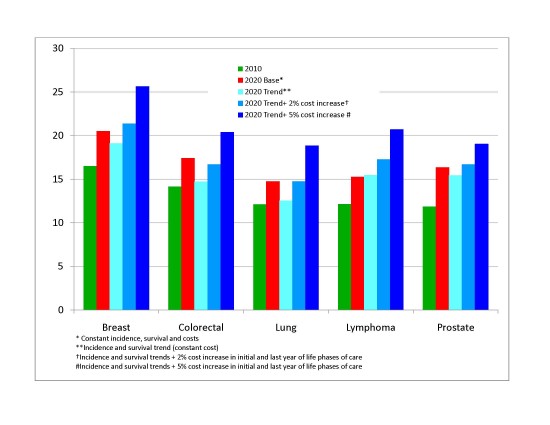
The projections were based on themost recent data available on cancer incidence, survival, and costs of care. In 2010, medical costs associated with cancer were projected to reach $124.6 billion, with the highest costs associated with breast cancer ($16.5 billion), followed by colorectal cancer ($14 billion), lymphoma ($12 billion), lung cancer ($12 billion) and prostate cancer ($12 billion).
If cancer incidence and survival rates and costs remain stable and the U.S. population ages at the rate predicted by the U.S. Census Bureau, direct cancer care expenditures would reach $158 billion in 2020, the report said.
However, the researchers also did additional analyses to account for changes in cancer incidence and survival rates and for the likelihood that cancer care costs will increase as new technologies and treatments are developed. Assuming a 2 percent annual increase in medical costs in the initial and final phases of care – which would mirror recent trends – the projected 2020 costs increased to $173 billion. Estimating a 5 percent annual increase in these costs raised the projection to $207 billion. These figures do not include other types of costs, such as lost productivity, which add to the overall financial burden of cancer.
“Rising health care costs pose a challenge for policy makers charged with allocating future resources on cancer research, treatment, and prevention,” said study author Angela Mariotto, Ph.D., from NCI’s Surveillance Research Program. “Because it is difficult to anticipate future developments of cancer control technologies and their impact on the burden of cancer, we evaluated a variety of possible scenarios.”
To project national cancer expenditures, the researchers combined cancer prevalence, which is the current number of people living with cancer, with average annual costs of care by age (less than 65 or 65 and older). According to their prevalence estimates, there were 13.8 million cancer survivors alive in 2010, 58 percent of whom were age 65 or older. If cancer incidence and survival rates remain stable, the number of cancer survivors in 2020 will increase by 31 percent, to about 18.1 million. Because of the aging of the U.S. population, the researchers expect the largest increase in cancer survivors over the next 10 years to be among Americans age 65 and older.
“The rising costs of cancer care illustrate how important it is for us to advance the science of cancer prevention and treatment to ensure that we’re using the most effective approaches,” said Robert Croyle, Ph.D., director, Division of Cancer Control and Population Sciences, NCI. “This is especially important for elderly cancer patients with other complex health problems.”
To develop their cost projections, the authors used average medical costs for the different phases of cancer care: the first year after diagnosis, the last year of life, and the time in between. For all types of cancer, per-person costs of care were highest in the final year of life. Per-person costs associated with the first year after a cancer diagnosis were more varied, with cancers of the brain, pancreas, ovaries, esophagus and stomach having the highest initial costs and melanoma, prostate and breast cancers having the lowest initial-year costs.
These new projections are higher than previously published estimates of direct cancer expenditures, largely because the researchers used the most recent data available — including Medicare claims data through 2006, which include payments for newer, more expensive, targeted therapies which attack specific cancer cells and often have fewer side effects than other types of cancer treatments. In addition, by analyzing costs according to phase of care, which revealed the higher costs of care associated with the first year of treatment and last year of life (for those who die from their disease), the researchers were able to generate more precise estimates of the cost of care.
The researchers used 2005 incidence and mortality data from NCI’s Surveillance, Epidemiology and End Results (SEER) program to estimate cancer prevalence for 2010 and 2020. Population estimates for the United States was obtained from the U.S. Census Bureau’s National Interim Projections for 2006 to 2020. Medical cost estimates were obtained using the SEER-Medicare database which links SEER data to Medicare claims data from the Center for Medicare and Medicaid Services.
——————————————————————————–
* More information about these cost projections is available at: http://costprojections.cancer.gov
** For more information about NCI’s Health Services and Economics Branch, please visit: http://healthservices.cancer.gov/
*** For more information about NCI’s Surveillance Research Program, please visit: http://surveillance.cancer.gov/
**** NCI leads the National Cancer Program and the NIH effort to dramatically reduce the burden of cancer and improve the lives of cancer patients and their families, through research into prevention and cancer biology, the development of new interventions, and the training and mentoring of new researchers. For more information about cancer, please visit the NCI Web site at www.cancer.gov or call NCI’s Cancer Information Service at 1-800-4-CANCER (1-800-422-6237).
***** The National Institutes of Health (NIH) — The Nation’s Medical Research Agency — includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. It is the primary federal agency for conducting and supporting basic, clinical and translational medical research, and it investigates the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
——————————————————————————–
Reference: Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, and Brown ML. Projections of the Cost of Cancer Care in the United States: 2010-2020. Jan 19, 2011, JNCI, Vol. 103, No. 2.
——————————————————————————–
Note: On January 13, 2011, a figure in the 2nd paragraph of this release was changed from $127.6 billion to the correct figure of $124.6 billion.
——————————————————————————–
Graph: Graf shows cost projections for breast cancer, colorectal cancer, lung cancer, lymphoma, and prostate cancer. There are five lines for each cancer. The first line represents 2010 costs, the second represents 2020 costs if incidence, survival, and costs remain constant, and the third line represents costs for 2020 if costs remains constant but incidence and survival mirror recent trends. The fourth and fifth lines represent costs if incidence and survival follow trends and costs increase by 2 percent, and 5 percent, respectively. The values on the graph are as follows (expressed as costs in US 2010 billion dollars): Breast 16.49982, 20.49625, 19.08418, 21.36733, 25.64077. Colorectal 14.14048, 17.40829, 14.69941, 16.68146, 20.39135. Lung, 12.1207, 14.73277, 12.53303, 14.73016, 18.8426. Lymphoma, 12.14254, 15.26053, 15.43801, 17.26625, 20.68822. Prostate, 11.84809, 16.34137, 15.40885, 16.66773, 19.02401



















