Artificial Human Liver May Speed Drug Development
Artificial Human Liver May Speed Drug Development
Scientists have devised an artificial human liver that, when implanted in mice, continues to make human proteins and break down certain drugs as the human liver would. The technique could lead to more accurate testing of potential medications.
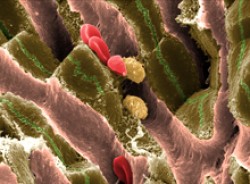
- A scanning electron micrograph reveals the complexities of mouse liver tissue, including hepatocytes (greenish brown) and red blood cells. Photo by EM Unit, UCL Medical School, Royal Free Campus. All rights reserved by Wellcome Images.
All experimental drugs must first be assessed in animals before they can be given to people. Mice are often used for such tests. But liver enzymes in mice differ from those in humans, and so vary in how they break down, or metabolize, drugs. As a result, experimental drugs that prove safe in mice may unexpectedly break down to create harmful metabolites in humans.
To avoid this obstacle, several research teams have been trying to “humanize” mice, sometimes by transplanting human liver cells into the animals. But for these techniques to work, the mouse’s own liver must be disabled, along with its immune system to avoid an attack on the transplanted human cells. With these methods, it may take weeks or months for the human liver cells to latch onto and expand in the mouse liver.
In the new study, Dr. Alice A. Chen of the Massachusetts Institute of Technology and her colleagues generated improved artificial human liver tissues that can begin functioning in mice in less than a week without harming their immune systems or liver. The research was supported in part by NIH’s National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute of Biomedical Imaging and Bioengineering (NIBIB) and National Cancer Institute (NCI).
To create the artificial liver, the scientists grew human liver cells, or hepatocytes, mixed with supportive mouse cells called fibroblasts. The cells were then encapsulated with human liver endothelial cells in a disc-shaped polymer scaffold. The endothelial cells secrete compounds that help keep hepatocytes alive and functioning, and the polymer gel scaffold protects against immune system attack. The method was described in the July 11, 2011, online early edition of the Proceedings of the National Academy of Sciences.
The researchers showed that when the liver tissue is implanted in the mouse body cavity, it becomes integrated into the animal’s circulatory system within a week. As a result, drugs can reach the liver, and human proteins produced by the liver can enter the bloodstream.
To test the function of the artificial livers, the scientists gave the mice drugs that are known to break down differently in humans. They found they were then able to detect drug byproducts that are normally generated only by human livers.
“The idea that you could take a humanized mouse and identify these metabolites before going to clinical trials is potentially very valuable,” Chen says. With further research, the technique might able to detect problematic drugs before they’re tested in humans. It might also aid the study of human liver disease and infections.
* The above story is reprinted from materials provided by National Institutes of Health (NIH)
** The National Institutes of Health (NIH) , a part of the U.S. Department of Health and Human Services, is the nation’s medical research agency—making important discoveries that improve health and save lives. The National Institutes of Health is made up of 27 different components called Institutes and Centers. Each has its own specific research agenda. All but three of these components receive their funding directly from Congress, and administrate their own budgets.



















