Swimming through the blood stream: Stanford engineers create wireless, self-propelled medical device
Swimming through the blood stream: Stanford engineers create wireless, self-propelled medical device
For 50 years, scientists searched for the secret to making tiny implantable devices that could travel through the bloodstream. Engineers at Stanford have demonstrated just such a device. Powered without wires or batteries, it can propel itself though the bloodstream and is small enough to fit through blood vessels.
…
Stanford electrical engineers have created a tiny wireless chip, driven by magnetic currents, that’s small enough to travel inside the human body. They hope it will be used for a wide range of biomedical applications, from delivering drugs to cleaning arteries.
…
Someday, your doctor may turn to you and say, “Take two surgeons and call me in the morning.” If that day arrives, you may have electrical engineer Ada Poon to thank.
This week, at the International Solid-State Circuits Conference, before an audience of her peers, Poon demonstrated a tiny, wirelessly powered, self-propelled medical device capable of controlled motion through a fluid – blood, to be exact. The era of swallow-the-surgeon medical care may no longer be the stuff of science fiction.
Poon, an assistant professor of electrical engineering, is developing a new class of medical devices that can be implanted or injected into the human body and powered wirelessly using electromagnetic radio waves. No batteries to wear out. No cables to provide power.
“Such devices could revolutionize medical technology,” said Poon. “Applications include everything from diagnostics to minimally invasive surgeries.”
Some of these new devices, like heart probes, chemical and pressure sensors, cochlear implants, pacemakers and drug pumps, would be stationary within the body. Others, like Poon’s most recent creations, could travel through the bloodstream to deliver drugs, perform analyses, and perhaps even zap blood clots or remove plaque from sclerotic arteries.
Challenged by power
The idea of implantable medical devices is not new, but most of today’s implements are challenged by the size of their batteries, which are large and heavy and must be replaced periodically. Fully half the volume of most of these devices is consumed by battery.
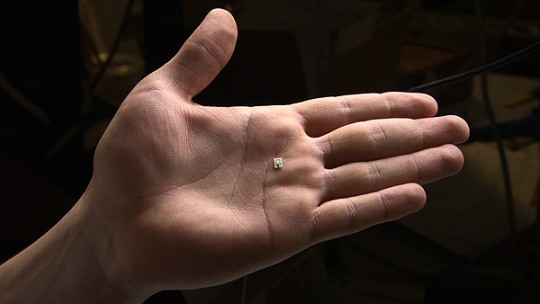 The current prototype chip, shown here resting on a hand, is only three millimeters wide and four millimeters long.
The current prototype chip, shown here resting on a hand, is only three millimeters wide and four millimeters long.
“While we have gotten very good at shrinking electronic and mechanical components of implants, energy storage has lagged in the move to miniaturize,” said co-author Teresa Meng, a professor of electrical engineering and computer science. “This hinders us in where we can place implants within the body and also creates the risk of corrosion or broken wires, not to mention replacing aging batteries.”
Poon’s devices are different. They consist of a radio transmitter outside the body sending signals inside the body to an independent device that picks up the signal with an antenna of coiled wire. The transmitter and the antennae are magnetically coupled such that any change in current flow in the transmitter produces a voltage in the other wire – or, more accurately, it induces a voltage. The power is transferred wirelessly. It can be used to run electronics on the device and propel it through the bloodstream.
Upending convention
It sounds easy, but it is not. Poon had to first upend some long-held assumptions about the delivery of wireless power inside the human body.
For 50 years, scientists have been working on wireless electromagnetic powering of implantable devices, but they ran up against mathematics. According to the models, high-frequency radio waves dissipate quickly in human tissue, fading exponentially the deeper they go.
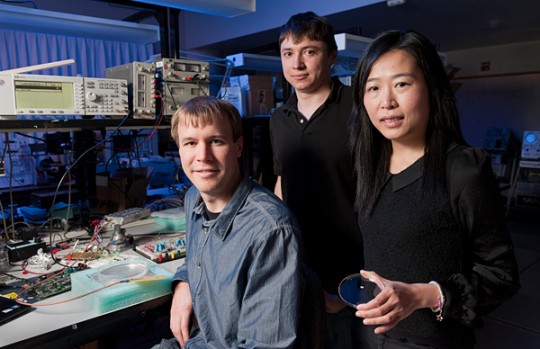 Professor Ada Poon, right, with graduate students Daniel Pivonka, left, and Anatoly Yakovlev, center. In the dish she is holding is the device that they created.
Professor Ada Poon, right, with graduate students Daniel Pivonka, left, and Anatoly Yakovlev, center. In the dish she is holding is the device that they created.
Low-frequency signals, on the other hand, penetrate well, but require antennae a few centimeters in diameter to provide enough power for the device, far too large to fit through any but the biggest arteries. In essence, because the math said it could not be done, the engineers never tried.
Then a curious thing happened. Poon started to look more closely at the models. She realized that scientists were approaching the problem incorrectly. In their models, they assumed that human muscle, fat and bone were generally good conductors of electricity, and therefore governed by a specific subset – the “quasi-static approximation,” to be exact – of the mathematical principles known as Maxwell’s equations.
Poon took a different tack, choosing instead to model tissue as a dielectric – a type of insulator.As it turns out, human tissue is a poor conductor of electricity. But radio waves can still move through tissue. In a dielectric, the signal is conveyed as waves of shifting polarization of atoms within cells. Even better, Poon also discovered that human tissue is a “low-loss” dielectric; that is, little of the signal gets lost along the way.
She recalculated using a different set of equations and made a surprising discovery: radio waves travel much farther in human tissue than originally thought.
Revelation
“When we extended things to higher frequencies using a simple model of tissue, we realized that the optimal frequency for wireless powering is actually around one gigahertz,” said Poon, “about 100 times higher than previously thought.”
More significantly, however, her revelation meant that antennae inside the body could be 100 times smaller and yet deliver the power needed by the medical device.
Poon was not so much in search of a new technology; she was in search of a new math. The antenna on the device Poon demonstrated at the conference is just 2 millimeters square, small enough to travel through the bloodstream.
She has developed two types of self-propelled devices. One drives electrical current directly through the fluid to create a directional force that pushes the device forward. This type of device is capable of moving at just over half-a-centimeter per second. The second type switches current back-and-forth through a wire loop to produce a swishing motion similar to the motion a kayaker makes to paddle upstream.
“There is considerable room for improvement and much work remains before such devices are ready for medical applications,” said Poon. “But for the first time in decades the possibility seems closer than ever.”
Stanford doctoral candidates Daniel Pivonka and Anatoly Yakovlev contributed to this research.
Ada Poon’s research was made possible by the support of C2S2 Focus Center, Olympus Corporation and Taiwan Semiconductor Manufacturing Company.
By Andrew Myers
Andrew Myers is associate director of communications for the Stanford School of Engineering
###
* Stanford University Medical Center integrates research, medical education and patient care at its three institutions – Stanford University School of Medicine, Stanford Hospital & Clinics and Lucile Packard Children’s Hospital.
** The above story is adapted from materials provided by Stanford University School of Medicine
________________________________________________________________




















