Study Points to Potential Treatment for Sickle Cell Disease
Study Points to Potential Treatment for Sickle Cell Disease
Scientists corrected sickle cell disease in adult laboratory mice by activating production of a special blood protein normally produced only before birth. The approach may lead to new treatments for people with the blood disorder.
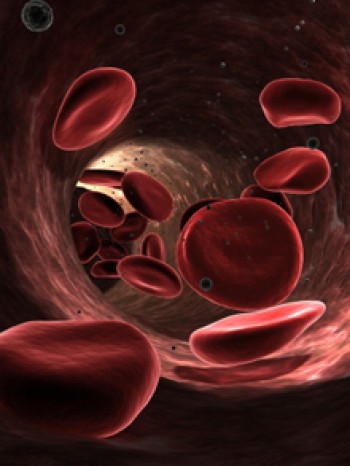 Sickle cell disease is caused by an abnormality in hemoglobin, the protein in red blood cells that carries oxygen throughout the body. About 100,000 Americans live with sickle cell disease. It is most prevalent in people of African, Hispanic, Mediterranean and Middle Eastern descent.
Sickle cell disease is caused by an abnormality in hemoglobin, the protein in red blood cells that carries oxygen throughout the body. About 100,000 Americans live with sickle cell disease. It is most prevalent in people of African, Hispanic, Mediterranean and Middle Eastern descent.
People with sickle cell disease have 2 copies of an altered hemoglobin gene. The defective protein that results changes shape after releasing its oxygen. This causes red blood cells to become stiff, misshapen and sticky. These sickle-shaped cells slow blood flow to tissues, resulting in organ damage.
There is no widely available cure for sickle cell disease. Bone marrow transplants have cured some patients. However, the treatment poses several risks, and most patients don’t have relatives who can donate compatible, healthy bone marrow.
Past studies have shown that an elevated level of a form of hemoglobin called fetal hemoglobin reduces the tendency of sickle hemoglobin to change the shape of red blood cells. Production of fetal hemoglobin normally predominates before birth but turns off as adult hemoglobin takes over. A drug called hydroxyurea can boost production of fetal hemoglobin and reduce the complications of sickle cell disease. However, not all patients respond well to this medication, and adverse side effects are a concern.
A research team led by Dr. Stuart Orkin set out to explore a more targeted approach to raising fetal hemoglobin by blocking production of a protein called BCL11A. The team—at Harvard Medical School, Children’s Hospital of Boston and the Howard Hughes Medical Institute, Boston—had previously demonstrated that BCL11A suppresses the production of fetal hemoglobin soon after birth. Their work was funded by NIH’s National Heart, Lung and Blood Institute (NHLBI), National Cancer Institute (NCI) and National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The study appeared in the October 13, 2011, online edition of Science.
The scientists used a genetic technique to inactivate the gene for BCL11A in mice with sickle cell disease. Without BCL11A, the mice continued to produce fetal hemoglobin. Sickled cells were absent in the mice, as were their disease symptoms. Other aspects of blood production appeared to be unaffected.
“This study provides the first proof of principle that BCL11A might serve as a target for treating sickle cell disease and related blood disorders such as the thalassemias,” Orkin says. More research is needed, however, before such therapies can be tested in people.
###
* The above story is reprinted from materials provided by National Institutes of Health (NIH)
** The National Institutes of Health (NIH) , a part of the U.S. Department of Health and Human Services, is the nation’s medical research agency—making important discoveries that improve health and save lives. The National Institutes of Health is made up of 27 different components called Institutes and Centers. Each has its own specific research agenda. All but three of these components receive their funding directly from Congress, and administrate their own budgets.



















