Bacteria Trigger Nerve Cells to Cause Pain
Bacteria Trigger Nerve Cells to Cause Pain
Researchers have found that bacteria can directly stimulate sensory neurons to produce pain and suppress inflammation. The finding may lead to better treatments for painful bacterial infections.
A tooth abscess, urinary tract infection, or other type of bacterial infection can cause intense pain. The pain is often accompanied by inflammation, which is produced by the immune system’s attack on the bacteria. It’s been thought that pain stems from immune cells, which release cytokines and growth factors that can induce inflammation and trigger sensory nerves.
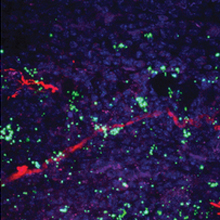
Bacteria (green) are found near neurons (red). Image by the researchers. Courtesy of Nature.
A team led by Drs. Isaac M. Chiu and Clifford J. Woolf at Boston Children’s Hospital sought to better understand the pain caused by bacterial infections. Their research was funded by NIH’s National Institute of Allergy and Infectious Diseases (NIAID), National Institute of Neurological Disorders and Stroke (NINDS), and Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).
The researchers used a mouse model of skin infection to study pain produced by the bacterium Staphylococcus aureus (S. aureus). Commonly known as “Staph,” these bacteria are a major cause of surgical infections. The study appeared on September 5, 2013, in Nature.
The team found that pain, as assessed by sensitivity of the mice to mechanical, heat and cold stimuli, didn’t correlate with tissue swelling or immune activation. Rather, pain correlated with the amount of bacteria present.
Mice in which immune pathways were blocked either had no difference or an increase in pain to a bacterial infection. This finding showed that the immune system wasn’t responsible for the pain from a bacterial infection.
To further examine the relationship between bacteria and pain, the team applied several strains of heat-killed bacteria directly to sensory neurons. The bacteria induced calcium fluxes and other changes in the neurons. The responses varied depending on the bacteria used, suggesting that differing mechanisms might be involved.
The researchers next tested various heat-stable molecules from bacteria. They found that sensory neurons could be activated by molecules called N-formyl peptides. A second heat-sensitive mechanism through which bacteria can cause pain, they found, is through a toxin called α-haemolysin, which forms pores in the membranes of target cells.
When sensory neurons and immune cells such as neutrophils and macrophages were placed together in cell culture, they formed close contacts. Experiments in mice showed that once sensory neurons are activated by bacteria, they release signals that suppress the immune system. These findings suggest that certain bacteria may have evolved to attack sensory neurons and thus hold back the immune system’s attack.
“We found that major parts of the immune system are not necessary for pain during infection, but that bacteria themselves are the source of much of the pain,” Chiu says. “If we could block pain in infected tissues and also block what pain neurons do to the immune system, it could help us treat bacterial infections better.”
By Carol Torgan, Ph.D.
###
* The above story is reprinted from materials provided by National Institutes of Health (NIH)
** The National Institutes of Health (NIH) , a part of the U.S. Department of Health and Human Services, is the nation’s medical research agency—making important discoveries that improve health and save lives. The National Institutes of Health is made up of 27 different components called Institutes and Centers. Each has its own specific research agenda. All but three of these components receive their funding directly from Congress, and administrate their own budgets.




















