Fungal Findings
Fungal Findings
A genomic survey of the fungi living on our skin provides a framework for understanding how these microbes contribute to skin health and disease.
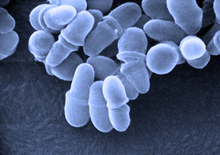
Malassezia fungi. Credit: Janice Haney Carr, CDC.
Complex communities of microbes live on the surface of our bodies. These fungi, bacteria and viruses are collectively known as the skin microbiome. A team from NIH’s National Human Genome Research Institute (NHGRI) and National Cancer Institute (NCI) previously used genomic techniques to study skin bacteria. They found diverse bacterial communities that varied between people and by skin site. In their new study, the team used a similar genomic approach to gain a better understanding of the fungi that live on our skin.
Fungi include molds, mushrooms, and the yeast that are used to ferment bread and beer. These microbes have been associated with many skin diseases and conditions, including athlete’s foot, eczema, dandruff and toenail infections. Fungal skin infections affect an estimated 29 million people nationwide. But fungi can be slow and difficult to grow in laboratories, making fungal infections hard to identify and treat.
As described online in Nature on May 22, 2013, the scientists collected samples at 14 body sites from 10 healthy adults. They focused on a fragment of DNA shared by all fungi—the intervening internal transcribed spacer 1 (ITS1) of ribosomal RNA—that could be used to classify fungi at the genus level with greater than 97% accuracy.
By generating more than 5 million ITS1 sequences from the samples, the team was able to identify more than 80 genus-level fungal types living on human skin. In contrast, traditional culturing methods could identify only 18 types. Ascomycetes and Basidiomycetes were found at all the skin sites. Fungi of the genus Malassezia were the predominant type on 11 of the 14 sites, including behind the ears, in nostrils, on the back, and on the arms.
The team found that heels, which don’t show extensive bacterial diversity, were the most complex site for fungi, with about 80 types represented. Toe webs, with about 60 types, and toenails, with 40, had the next highest levels of fungal diversity. Hands and arms, which harbor a great diversity of bacteria, had relatively few types of fungi. Fungal communities on the core body were quite stable over time, with little change when tested up to 3 months apart. In contrast, fungi on the feet altered considerably over 3 months, perhaps reflecting more environmental exposure.
“The fungal communities on the human body are complex and site-specific,” says co-senior author Dr. Heidi Kong of NCI. “By gaining a more complete awareness of the fungal and bacterial ecosystems, we can better address associated skin diseases, including fungal infections, which can be related to cancer treatments.”
“The data from our study gives us a baseline about normal individuals that we never had before,” says co-senior author Dr. Julie Segre of NHGRI. “The bottom line is your feet are teeming with fungal diversity, so wear your flip flops in locker rooms if you don’t want to mix your foot fungi with someone else’s fungi.”
* The above story is reprinted from materials provided by National Institutes of Health (NIH)
** The National Institutes of Health (NIH) , a part of the U.S. Department of Health and Human Services, is the nation’s medical research agency—making important discoveries that improve health and save lives. The National Institutes of Health is made up of 27 different components called Institutes and Centers. Each has its own specific research agenda. All but three of these components receive their funding directly from Congress, and administrate their own budgets.




















